Childhood Thymoma and Thymic Carcinoma Treatment (PDQ®): Treatment - Patient Information [NCI]
This information is produced and provided by the National Cancer Institute (NCI). The information in this topic may have changed since it was written. For the most current information, contact the National Cancer Institute via the Internet web site at http://cancer.gov or call 1-800-4-CANCER.
General Information About Thymoma and Thymic Carcinoma
Thymoma and thymic carcinoma are diseases in which malignant (cancer) cells form in the thymus.
Thymoma and thymic carcinoma are two types of cancer that can form in the cells that cover the outside surface of the thymus. The thymus is a small organ in the upper chest under the breastbone. It is part of the lymph system and makes white blood cells, called lymphocytes, that help fight infection. These cancers usually form between the lungs in the front part of the chest and are often found during a chest x-ray that is done for another reason.
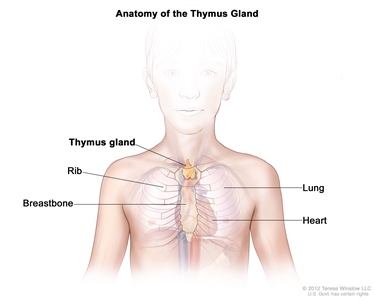
Anatomy of the thymus gland. The thymus gland is a small organ that lies in the upper chest under the breastbone. It makes white blood cells, called lymphocytes, which protect the body against infections.
Even though thymoma and thymic carcinoma form in the same type of cell, they act differently:
- Thymoma. The cancer cells look a lot like the normal cells of the thymus, grow slowly, and rarely spread beyond the thymus. A thymoma may become a thymic carcinoma over time.
- Thymic carcinoma. The cancer cells do not look like the normal cells of the thymus, grow more quickly, and are more likely to spread to other parts of the body.
Other types of tumors, such as lymphoma or germ cell tumors, may form in the thymus, but they are not considered to be thymoma or thymic carcinoma.
Signs and symptoms of thymoma and thymic carcinoma include coughing and trouble breathing.
These and other signs and symptoms may be caused by thymoma and thymic carcinoma or by other conditions.
Check with your child's doctor if your child has any of the following:
- Coughing.
- Trouble breathing.
- Pain or a tight feeling in the chest.
- Trouble swallowing.
- Hoarseness.
- Fever.
- Weight loss.
- Superior vena cava syndrome.
Children with thymoma or thymic carcinoma may also have other health problems.
Children who have thymoma or thymic carcinoma may also have one of the following immune system diseases or hormone disorders:
- Myasthenia gravis.
- Pure red cell aplasia.
- Hypogammaglobulinemia.
- Nephrotic syndrome.
- Scleroderma.
- Dermatomyositis.
- Lupus.
- Rheumatoid arthritis.
- Thyroiditis.
- Hyperthyroidism.
- Addison disease.
- Panhypopituitarism.
Tests that examine the thymus and chest are used to help diagnose thymoma and thymic carcinoma.
The following tests and procedures may be used:
- Physical exam and health history: An exam of the body to check general signs of health, including checking for signs of disease, such as lumps or anything else that seems unusual. A history of the patient's health habits and past illnesses and treatments will also be taken.
- Chest x-ray: An x-ray of the organs and bones inside the chest. An x-ray is a type of energy beam that can go through the body and onto film, making a picture of areas inside the body.
- CT scan (CAT scan): A procedure that makes a series of detailed pictures of areas inside the body, taken from different angles. The pictures are made by a computer linked to an x-ray machine. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography.
- MRI (magnetic resonance imaging): A procedure that uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body. This procedure is also called nuclear magnetic resonance imaging (NMRI).
- PET scan (positron emission tomography scan): A procedure to find malignant tumor cells in the body. A small amount of radioactive glucose (sugar) is injected into a vein. The PET scanner rotates around the body and makes a picture of where glucose is being used in the body. Malignant tumor cells show up brighter in the picture because they are more active and take up more glucose than normal cells do.
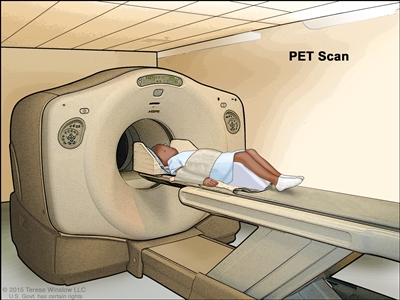
Positron emission tomography (PET) scan. The child lies on a table that slides through the PET scanner. The head rest and white strap help the child lie still. A small amount of radioactive glucose (sugar) is injected into the child's vein, and a scanner makes a picture of where the glucose is being used in the body. Cancer cells show up brighter in the picture because they take up more glucose than normal cells do. - Biopsy: The removal of cells or tissues so they can be viewed under a microscope by a pathologist to check for signs of cancer.
Certain factors affect prognosis (chance of recovery).
The prognosis depends on the following:
- Whether the cancer is thymoma or thymic carcinoma.
- Whether the cancer has spread to nearby areas or other parts of the body.
- Whether the cancer was completely removed by surgery.
- Whether the cancer is newly diagnosed or has recurred (come back) after treatment.
The prognosis is better when the cancer has not spread to other parts of the body. Childhood thymoma is usually diagnosed before the tumor has spread.
Stages of Thymoma and Thymic Carcinoma
After thymoma or thymic carcinoma has been diagnosed, tests are done to find out if cancer cells have spread to nearby areas or to other parts of the body.
The process used to find out if thymoma or thymic carcinoma has spread from the thymus to nearby areas or other parts of the body is called staging. Thymoma and thymic carcinoma may spread to the lungs, liver, kidneys, or the lining around the lungs and heart. The results of tests and procedures done to diagnose thymoma or thymic carcinoma are used to help make decisions about treatment.
Sometimes childhood thymoma or thymic carcinoma recurs (comes back) after treatment.
There are three ways that cancer spreads in the body.
Cancer can spread through tissue, the lymph system, and the blood:
- Tissue. The cancer spreads from where it began by growing into nearby areas.
- Lymph system. The cancer spreads from where it began by getting into the lymph system. The cancer travels through the lymph vessels to other parts of the body.
- Blood. The cancer spreads from where it began by getting into the blood. The cancer travels through the blood vessels to other parts of the body.
Cancer may spread from where it began to other parts of the body.
When cancer spreads to another part of the body, it is called metastasis. Cancer cells break away from where they began (the primary tumor) and travel through the lymph system or blood.
- Lymph system. The cancer gets into the lymph system, travels through the lymph vessels, and forms a tumor (metastatic tumor) in another part of the body.
- Blood. The cancer gets into the blood, travels through the blood vessels, and forms a tumor (metastatic tumor) in another part of the body.
The metastatic tumor is the same type of cancer as the primary tumor. For example, if thymic carcinoma spreads to the lung, the cancer cells in the lung are actually thymic carcinoma cells. The disease is metastatic thymic carcinoma, not lung cancer.
Treatment Option Overview
There are different types of treatment for children with thymoma or thymic carcinoma.
Some treatments are standard (the currently used treatment), and some are being tested in clinical trials. A treatment clinical trial is a research study meant to help improve current treatments or obtain information on new treatments for patients with cancer. When clinical trials show that a new treatment is better than the standard treatment, the new treatment may become the standard treatment.
Because cancer in children is rare, taking part in a clinical trial should be considered. Some clinical trials are open only to patients who have not started treatment.
Children with thymoma or thymic carcinoma should have their treatment planned by a team of doctors who are experts in treating childhood cancer.
Treatment will be overseen by a pediatric oncologist, a doctor who specializes in treating children with cancer. The pediatric oncologist works with other pediatric health professionals who are experts in treating children with cancer and who specialize in certain areas of medicine. This may include the following specialists and others:
- Pediatrician.
- Pediatric surgeon.
- Radiation oncologist.
- Pathologist.
- Pediatric nurse specialist.
- Social worker.
- Rehabilitation specialist.
- Psychologist.
- Child-life specialist.
Five types of standard treatment are used:
Surgery
Surgery to remove the cancer is the main treatment for thymoma and thymic carcinoma. However, thymic carcinoma can rarely be completely removed by surgery and is likely to recur (come back) after treatment.
Radiation therapy
Radiation therapy is a cancer treatment that uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing. External radiation therapy uses a machine outside the body to send radiation toward the area of the body with cancer.
Chemotherapy
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body (systemic chemotherapy).
Hormone therapy
Hormone therapy is a cancer treatment that removes hormones or blocks their action and stops cancer cells from growing. Hormones are substances that are made by glands in the body and flow through the bloodstream. Some hormones can cause certain cancers to grow. If tests show that the cancer cells have places where hormones can attach (receptors), drugs may be used to reduce the production of hormones or block them from working. Hormone therapy using corticosteroids or octreotide may be used to treat thymoma.
Targeted therapy
Targeted therapy is a type of treatment that uses drugs or other substances to identify and attack specific cancer cells. Targeted therapies usually cause less harm to normal cells than chemotherapy or radiation therapy do.
- Tyrosine kinase inhibitors: These targeted therapy drugs block signals needed for tumors to grow. Sunitinib is used to treat thymoma and thymic carcinoma that did not respond to other treatments.
Targeted therapy is being studied for the treatment of thymoma and thymic carcinoma that has recurred (come back).
New types of treatment are being tested in clinical trials.
Information about clinical trials is available from the NCI website.
Treatment of thymoma and thymic carcinoma may cause side effects.
To learn more about side effects that begin during treatment for cancer, visit Side Effects.
Side effects from cancer treatment that begin after treatment and continue for months or years are called late effects. Late effects of cancer treatment may include:
- Physical problems.
- Changes in mood, feelings, thinking, learning, or memory.
- Second cancers (new types of cancer) or other conditions.
Some late effects may be treated or controlled. It is important to talk with your child's doctors about the possible late effects caused by some treatments. See the PDQ summary on Late Effects of Treatment for Childhood Cancer for more information.
Patients may want to think about taking part in a clinical trial.
For some patients, taking part in a clinical trial may be the best treatment choice. Clinical trials are part of the cancer research process. Clinical trials are done to find out if new cancer treatments are safe and effective or better than the standard treatment.
Many of today's standard treatments for cancer are based on earlier clinical trials. Patients who take part in a clinical trial may receive the standard treatment or be among the first to receive a new treatment.
Patients who take part in clinical trials also help improve the way cancer will be treated in the future. Even when clinical trials do not lead to effective new treatments, they often answer important questions and help move research forward.
Patients can enter clinical trials before, during, or after starting their cancer treatment.
Some clinical trials only include patients who have not yet received treatment. Other trials test treatments for patients whose cancer has not gotten better. There are also clinical trials that test new ways to stop cancer from recurring (coming back) or reduce the side effects of cancer treatment.
Clinical trials are taking place in many parts of the country. Information about clinical trials supported by NCI can be found on NCI's clinical trials search webpage. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
Follow-up tests may be needed.
As your child goes through treatment, they will have follow-up tests or check-ups. Some tests that were done to diagnose or stage the cancer may be repeated to see how well the treatment is working. Decisions about whether to continue, change, or stop treatment may be based on the results of these tests.
Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your child's condition has changed or if the cancer has recurred (come back).
Treatment of Thymoma
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of newly diagnosed thymoma may include the following:
- Surgery to remove as much of the tumor as possible.
- Radiation therapy, for tumors that cannot be removed by surgery or if tumor remains after surgery.
- Chemotherapy, for tumors that did not respond to other treatments.
- Hormone therapy (octreotide), for tumors that did not respond to other treatments.
- Targeted therapy (sunitinib), for tumors that did not respond to other treatments.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Thymic Carcinoma
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of newly diagnosed thymic carcinoma may include the following:
- Surgery to remove as much of the tumor as possible.
- Radiation therapy, for tumors that cannot be removed by surgery or if tumor remains after surgery.
- Chemotherapy, for tumors that did not respond to radiation therapy.
- Targeted therapy (sunitinib), for tumors that did not respond to other treatments.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Recurrent Thymoma and Thymic Carcinoma
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of recurrent thymoma and thymic carcinoma in children may include the following:
- A clinical trial that checks a sample of the patient's tumor for certain gene changes. The type of targeted therapy that will be given to the patient depends on the type of gene change.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
To Learn More About Thymoma and Thymic Carcinoma
For more information from the National Cancer Institute about childhood thymoma and thymic carcinoma, see the following:
- Thymoma and Thymic Carcinoma Home Page
- Computed Tomography (CT) Scans and Cancer
- Targeted Cancer Therapies
For more childhood cancer information and other general cancer resources, visit:
- About Cancer
- Childhood Cancers
- CureSearch for Children's Cancer
- Late Effects of Treatment for Childhood Cancer
- Adolescents and Young Adults with Cancer
- Children with Cancer: A Guide for Parents
- Cancer in Children and Adolescents
- Cancer Staging
- Coping with Cancer
- Questions to Ask Your Doctor about Cancer
- For Survivors, Caregivers, and Advocates
About This PDQ Summary
About PDQ
Physician Data Query (PDQ) is the National Cancer Institute's (NCI's) comprehensive cancer information database. The PDQ database contains summaries of the latest published information on cancer prevention, detection, genetics, treatment, supportive care, and complementary and alternative medicine. Most summaries come in two versions. The health professional versions have detailed information written in technical language. The patient versions are written in easy-to-understand, nontechnical language. Both versions have cancer information that is accurate and up to date and most versions are also available in Spanish.
PDQ is a service of the NCI. The NCI is part of the National Institutes of Health (NIH). NIH is the federal government's center of biomedical research. The PDQ summaries are based on an independent review of the medical literature. They are not policy statements of the NCI or the NIH.
Purpose of This Summary
This PDQ cancer information summary has current information about the treatment of childhood thymoma and thymic carcinoma. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Reviewers and Updates
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary ("Updated") is the date of the most recent change.
The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Pediatric Treatment Editorial Board.
Clinical Trial Information
A clinical trial is a study to answer a scientific question, such as whether one treatment is better than another. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in order to find new and better ways to help cancer patients. During treatment clinical trials, information is collected about the effects of a new treatment and how well it works. If a clinical trial shows that a new treatment is better than one currently being used, the new treatment may become "standard." Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Clinical trials can be found online at NCI's website. For more information, call the Cancer Information Service (CIS), NCI's contact center, at 1-800-4-CANCER (1-800-422-6237).
Permission to Use This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely as text. It cannot be identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as "NCI's PDQ cancer information summary about breast cancer prevention states the risks in the following way: [include excerpt from the summary]."
The best way to cite this PDQ summary is:
PDQ® Pediatric Treatment Editorial Board. PDQ Childhood Thymoma and Thymic Carcinoma Treatment. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/types/thymoma/patient/child-thymoma-treatment-pdq. Accessed <MM/DD/YYYY>.
Images in this summary are used with permission of the author(s), artist, and/or publisher for use in the PDQ summaries only. If you want to use an image from a PDQ summary and you are not using the whole summary, you must get permission from the owner. It cannot be given by the National Cancer Institute. Information about using the images in this summary, along with many other images related to cancer can be found in Visuals Online. Visuals Online is a collection of more than 3,000 scientific images.
Disclaimer
The information in these summaries should not be used to make decisions about insurance reimbursement. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website's E-mail Us.
Last Revised: 2020-09-28
If you want to know more about cancer and how it is treated, or if you wish to know about clinical trials for your type of cancer, you can call the NCI's Cancer Information Service at 1-800-422-6237, toll free. A trained information specialist can talk with you and answer your questions.