Cervical Cancer Treatment: Treatment - Patient Information [NCI]
This information is produced and provided by the National Cancer Institute (NCI). The information in this topic may have changed since it was written. For the most current information, contact the National Cancer Institute via the Internet web site at http://cancer.gov or call 1-800-4-CANCER.
What Is Cervical Cancer?
Cervical cancer is cancer that starts in the cells of the cervix. The cervix is the lower, narrow end of the uterus (womb). The cervix connects the uterus to the vagina (birth canal). Cervical cancer usually develops slowly over time. Before cancer appears in the cervix, the cells of the cervix go through changes known as dysplasia, in which abnormal cells begin to appear in the cervical tissue. Over time, if not destroyed or removed, the abnormal cells may become cancer cells and start to grow and spread more deeply into the cervix and to surrounding areas.
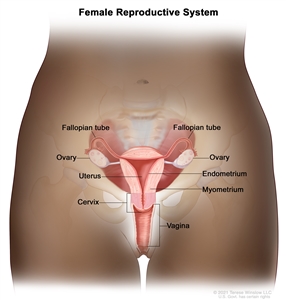
Anatomy of the female reproductive system. The organs in the female reproductive system include the uterus, ovaries, fallopian tubes, cervix, and vagina. The uterus has a muscular outer layer called the myometrium and an inner lining called the endometrium.
The cervix has two main parts:
- The ectocervix (also called exocervix) is the outer part of the cervix that can be seen during a gynecologic exam. The ectocervix is covered with thin, flat cells called squamous cells.
- The endocervix is the inner part of the cervix that forms a canal that connects the vagina to the uterus. The endocervix is covered with column-shaped glandular cells that make mucus.
The squamocolumnar junction (also called the transformation zone) is the border where the endocervix and ectocervix meet. Most cervical cancers begin in this area.
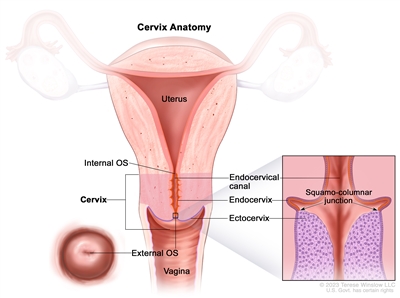
Anatomy of the cervix. The cervix is the lower, narrow end of the uterus that connects the uterus to the vagina. It is made up of the internal OS (the opening between the cervix and the upper part of the uterus), the endocervix (the inner part of the cervix that forms the endocervical canal), the ectocervix (the outer part of the cervix that opens into the vagina) and the external OS (the opening between the cervix and vagina). The area where the endocervix and ectocervix meet is called the squamocolumnar junction, which contains both glandular cells (column-shaped cells that make mucus) from the endocervix and squamous cells (thin, flat cells) from the ectocervix. The squamocolumnar junction is sometimes referred to as the transformation zone.
Types of cervical cancer
Cervical cancers are named after the type of cell where the cancer started. The two main types are:
- Squamous cell carcinoma: Most cervical cancers (up to 90%) are squamous cell carcinomas. These cancers develop from cells in the ectocervix.
- Adenocarcinoma: Cervical adenocarcinomas develop in the glandular cells of the endocervix. Clear cell adenocarcinoma, also called clear cell carcinoma or mesonephroma, is a rare type of cervical adenocarcinoma.
Sometimes, cervical cancer has features of both squamous cell carcinoma and adenocarcinoma. This is called mixed carcinoma or adenosquamous carcinoma. Very rarely, cancer develops in other cells in the cervix.
Learn more about cervical cancer
Many cervical cancer symptoms are also seen with other, less serious conditions. These are the warning signs you shouldn't ignore.
Causes, Risk Factors, and Prevention
Long-lasting HPV infection causes almost all cervical cancers. Learn about HPV infection and other risk factors for cervical cancer and what you can do to lower your risk.
If you have a cervix, screening for cervical cancer is an important part of routine health care. Learn when to get screened and what to expect during and after screening.
Learn what HPV and Pap test results mean and next steps if a test result is abnormal.
Learn about the tests that are used to diagnose and stage cervical cancer.
Learn about cervical cancer survival rates and why this statistic doesn't predict exactly what will happen to you.
Stage refers to the extent of your cancer, such as how large the tumor is and if it has spread. Learn about cervical cancer stages, an important factor in deciding your treatment plan.
Learn about the different ways cervical cancer can be treated.
Childhood Cervical and Vaginal Cancers
Cervical cancer and vaginal cancer are very rare in children. Learn about the signs and symptoms, diagnosis, and treatment options.
Certain aspects of cervical cancer diagnosis and treatment are of special concern. Gain a greater sense of control by knowing what to expect and what resources are available to help you cope.
Cervical Cancer Symptoms
Early on, cervical cancer usually doesn't have symptoms, making it hard to detect. Symptoms usually begin after the cancer has spread.
When symptoms of early-stage cervical cancer do occur, they may include
- vaginal bleeding after sex
- vaginal bleeding after menopause
- vaginal bleeding between periods or periods that are heavier or longer than normal
- vaginal discharge that is watery and has a strong odor or that contains blood
- pelvic pain or pain during sex
Symptoms of advanced cervical cancer (cancer has spread beyond the cervix to other parts of the body) may include the symptoms of early-stage cervical cancer and
- difficult or painful bowel movements or bleeding from the rectum when having a bowel movement
- difficult or painful urination or blood in the urine
- dull backache
- swelling of the legs
- pain in the abdomen
- feeling tired
These symptoms may be caused by many conditions other than cervical cancer. The only way to know is to see a health professional. If it is cervical cancer, ignoring symptoms can delay treatment and make it less effective.
Learn how cervical cancer screening can help prevent cervical cancer or find it early.
Cervical Cancer Diagnosis
If you have symptoms or screening test results that suggest the possibility of cervical cancer, your doctor will do follow-up tests to find out if it is due to cancer or some other cause. They will usually start by asking about your personal and family medical history and by doing a physical exam, which will include a pelvic exam and rectovaginal exam. They may recommend diagnostic tests to find out if you have cervical cancer, and if so, whether it has spread to another part of the body. The results of these tests will also help you and your doctor plan treatment.
How cervical cancer is diagnosed
The following procedures are used to diagnose cervical cancer:
Colposcopy
Colposcopy is a procedure in which the health care provider inserts a speculum to gently open the vagina and view the cervix. A vinegar solution will be applied to the cervix to help show abnormal areas. The health care provider then places an instrument called a colposcope close to the vagina. It has a bright light and a magnifying lens and allows the health care provider to look closely at the cervix. A colposcopy usually includes a biopsy.
Biopsy
Biopsy is a procedure in which a sample of tissue is removed from the cervix so that a pathologist can view it under a microscope to check for signs of cancer. The following types of biopsies are used to check for cervical cancer:
- Punch biopsy is a procedure in which a small, round piece of tissue is removed using a sharp, hollow circular instrument. Sometimes several different areas of the cervix will be checked with punch biopsy. This procedure is usually done in the doctor's office.
- Endocervical curettage is a procedure to collect cells or tissue from the cervical canal using a curette (spoon-shaped instrument). This procedure removes only a small amount of tissue and is usually done in the doctor's office.
- Loop electrosurgical excision procedure (LEEP) uses a thin wire loop, through which an electrical current is passed, to remove tissue from the cervix. LEEP may be used to diagnose cervical cancer. It also may be used to remove precancer or early-stage cancer. This procedure is typically done in a doctor's office. It usually takes only a few minutes, and local anesthesia is used to numb the area.
- Cone biopsy is surgery to remove a larger, cone-shaped piece of tissue from the cervix and cervical canal. A cone biopsy may be used to diagnose cervical cancer. It also may be used to remove precancer or early-stage cancer. This procedure is also called conization. A cone biopsy is done at the hospital under general anesthesia.
Talk with your health care provider to learn what to expect during and after your biopsy procedure. Some people have bleeding and/or discharge after a biopsy. Others have pain that feels like cramps during menstruation.
To learn about the type of information that can be found in a pathologist's report about the cells or tissue removed during a biopsy, see Pathology Reports.
Tests and procedures used to stage cervical cancer
If you are diagnosed with cervical cancer, you will be referred to a gynecologic oncologist. This is a doctor who specializes in staging and treating cervical cancer and other cancers of the female reproductive system. They will recommend tests to determine the extent (stage) of cancer. Sometimes the cancer is only in the cervix. Or, it may have spread from the cervix to other parts of the body. The process of learning the extent of cancer in the body is called staging. It is important to know the stage of the cervical cancer in order to plan the best treatment.
For information about a specific stage of cervical cancer, see Cervical Cancer Stages.
The following procedures may be used to determine the cervical cancer stage:
Imaging tests
- PET-CT scan combines the pictures from a positron emission tomography (PET) scan and a computed tomography (CT) scan. The PET and CT scans are done at the same time on the same machine. The pictures from both scans are combined to make a more detailed picture than either test would make by itself.
- For the PET scan, a small amount of radioactive glucose (sugar) is injected into a vein. The scanner rotates around the body and makes a picture of where glucose is being used in the body. Malignant tumor cells show up brighter in the picture because they are more active and take up more glucose than normal cells.
- For the CT scan, a series of detailed x-ray pictures of areas inside the body is taken from different angles. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly.
- Magnetic resonance imaging (MRI) uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body. This procedure is also called nuclear magnetic resonance imaging.
- Ultrasound uses high-energy sound waves (ultrasound), which bounce off internal tissues or organs and make echoes. The echoes form a picture of body tissues called a sonogram.
- Chest x-ray is an x-ray of the organs and bones inside the chest. An x-ray is a type of high-energy radiation that can go through the body and onto film, making a picture of areas inside the chest.
Lab tests
- Complete blood count (CBC) is a blood test that measures the following in a sample of blood:
- the number of red blood cells, white blood cells, and platelets
- the amount of hemoglobin (the protein that carries oxygen) in the red blood cells
- the portion of the blood sample made up of red blood cells
- Blood chemistry study is a blood test that measures the amounts of certain substances released into the blood by organs and tissues in the body, including electrolytes, lactate dehydrogenase, uric acid, blood urea nitrogen, creatinine, and liver function values. An unusual (higher or lower than normal) amount of a substance can be a sign of cancer spread or other diseases.
Visual examination
- Cystoscopy is a procedure to look inside the bladder and urethra to check for abnormal areas. A cystoscope is inserted through the urethra into the bladder. A cystoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove tissue samples, which are checked under a microscope for signs of cancer.
- Sigmoidoscopy uses a sigmoidoscope to look inside the rectum and sigmoid (lower) colon for abnormal areas. A sigmoidoscope is inserted through the rectum into the sigmoid colon. A sigmoidoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove tissue samples, which are checked under a microscope for signs of cancer.
Getting a second opinion
Some people want to get a second opinion to confirm their cervical cancer diagnosis and treatment plan. If you choose to seek a second opinion, you will need to get important medical test results and reports from the first doctor to share with the second doctor. The second doctor will review the pathology report, slides, and scans before giving a recommendation. The doctor who gives the second opinion may agree with your first doctor, suggest changes or another approach, or provide more information about your cancer.
For questions you might want to ask at your appointments, see Questions to Ask Your Doctor.
To learn more about choosing a doctor and getting a second opinion, see Finding Cancer Care. You can also contact NCI's Cancer Information Service via chat, email, or phone (both in English and Spanish) for help finding a doctor, hospital, or getting a second opinion.
Cervical Cancer Prognosis and Survival Rates
If you have been diagnosed with cervical cancer, you may have questions about how serious the cancer is and your chances of survival. The likely outcome or course of a disease is called prognosis.
The prognosis for cervical cancer depends on many factors:
- the stage of the cancer (the size of the tumor and whether the cancer has spread beyond the cervix)
- the type of cervical cancer (adenocarcinoma or squamous cell carcinoma)
- your age and general health
- whether you have other health problems or diseases, including if you are immunocompromised or have HIV
- whether the cancer is newly diagnosed or has recurred (come back)
Survival rates for cervical cancer
Doctors estimate cervical cancer prognosis by using statistics collected over many years from people with cervical cancer. One statistic that is commonly used in making a prognosis is the 5-year relative survival rate. The 5-year relative survival rate tells you what percent of people with the same type and stage of cervical cancer are alive 5 years after their cancer was diagnosed, compared with people in the overall population. For example, the 5-year relative survival rate for cervical cancer diagnosed at an early stage is 91%. This means that people diagnosed with early-stage cervical cancer are 91% as likely as people who do not have cervical cancer to be alive 5 years after diagnosis. The 5-year relative survival rates for cervical cancer are as follows:
- When cervical cancer is diagnosed at an early stage, the 5-year relative survival rate is 91%.
- When cervical cancer is diagnosed after it has spread to nearby tissues, organs, or regional lymph nodes, the 5-year relative survival rate is 60%.
- When cervical cancer is diagnosed after it has spread to a distant part of the body, the 5-year relative survival rate is 19%.
- The 5-year relative survival rate for all people with cervical cancer is 67%.
Learn more about statistics for cervical cancer, from our Cancer Stat Facts Collection.
Understanding survival rate statistics
Because prognosis statistics are based on large groups of people, they cannot be used to predict exactly what will happen to you. The doctor who knows the most about your situation is in the best position to discuss these statistics and talk with you about your prognosis. It is important to note the following when reviewing survival statistics:
- No two people are entirely alike, and responses to treatment can vary greatly.
- Survival statistics use information collected from large groups of people who may have received different types of treatment.
- It takes several years to see the effect of newer and better treatments, so these effects may not be reflected in current survival statistics.
To learn more about survival statistics and to see videos of patients and their doctors exploring their feelings about prognosis, see Understanding Cancer Prognosis.
Cervical Cancer Stages
A cancer stage describes the extent of cancer in the body, especially whether the cancer has spread from where it first formed to other parts of the body. It is important to know the stage of cervical cancer in order to plan the best treatment.
The International Federation of Gynecology and Obstetrics staging system is used for cervical cancer. Learn about tests and procedures used to determine the stage of cervical cancer.
Stage I cervical cancer
In stage I, cervical cancer has formed and is found in the cervix only. It is divided into stages IA and IB, based on the size of the tumor and the deepest point of tumor invasion.
Stage IA is subdivided based on the deepest point of tumor invasion. 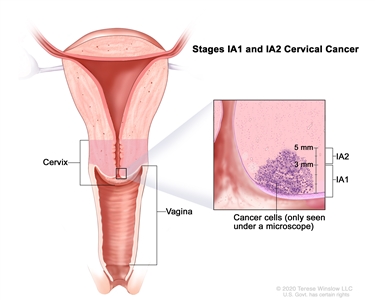
Stage IA1 and IA2 cervical cancer. A very small amount of cancer that can only be seen under a microscope is found in the tissues of the cervix. In stage IA1, the cancer is not more than 3 millimeters deep. In stage IA2, the cancer is more than 3 but not more than 5 millimeters deep.
- Stage IA1: A very small amount of cancer that can only be seen with a microscope is found in the tissues of the cervix. The deepest point of tumor invasion is 3 millimeters or less.
- Stage IA2: A very small amount of cancer that can only be seen with a microscope is found in the tissues of the cervix. The deepest point of tumor invasion is more than 3 millimeters but not more than 5 millimeters.
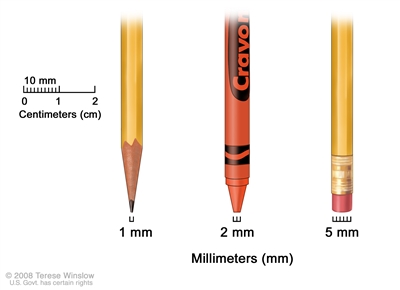
Millimeters (mm). A sharp pencil point is about 1 mm, a new crayon point is about 2 mm, and a new pencil eraser is about 5 mm.
Stage IB is subdivided based on the size of the tumor and the deepest point of tumor invasion.
- Stage IB1: The tumor is 2 centimeters or smaller and the deepest point of tumor invasion is more than 5 millimeters.
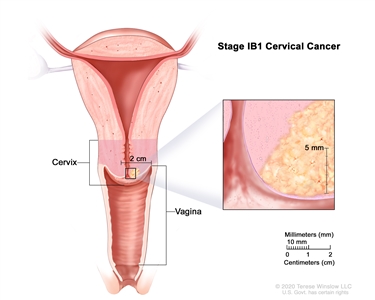
Stage IB1 cervical cancer. The cancer is 2 centimeters or smaller and is more than 5 millimeters deep. - Stage IB2: The tumor is larger than 2 centimeters but not larger than 4 centimeters.
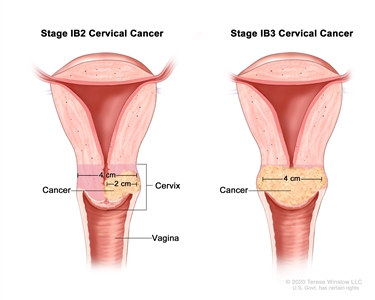
Stage IB2 and IB3 cervical cancer. In stage IB2, the cancer is larger than 2 centimeters but not larger than 4 centimeters. In stage IB3, the cancer is larger than 4 centimeters. - Stage IB3: The tumor is larger than 4 centimeters.
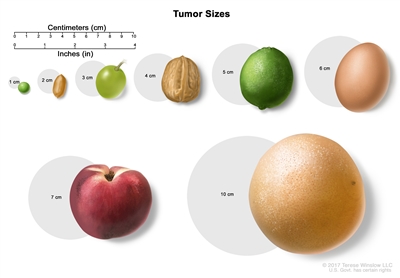
Tumor sizes are often measured in centimeters (cm) or inches. Common food items that can be used to show tumor size in cm include: a pea (1 cm), a peanut (2 cm), a grape (3 cm), a walnut (4 cm), a lime (5 cm or 2 inches), an egg (6 cm), a peach (7 cm), and a grapefruit (10 cm or 4 inches).
Learn about treatment of stage I cervical cancer.
Learn about treatment of cervical cancer during pregnancy.
Stage II cervical cancer
In stage II, cervical cancer has spread to the upper two-thirds of the vagina or to the tissue around the uterus.
Stage II is subdivided based on how far the cancer has spread. 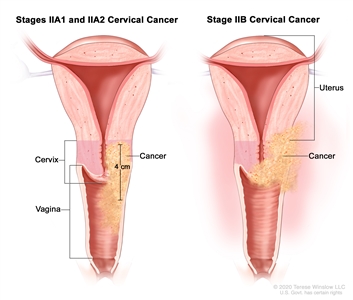
Stage II cervical cancer. In stages IIA1 and IIA2, cancer has spread from the cervix to the upper two-thirds of the vagina but has not spread to the tissue around the uterus. In stage IIA1, the cancer is 4 centimeters or smaller. In stage IIA2, the cancer is larger than 4 centimeters. In stage IIB, cancer has spread from the cervix to the tissue around the uterus.
- Stage IIA: Cancer has spread from the cervix to the upper two-thirds of the vagina but has not spread to the tissue around the uterus. Stage IIA is further divided based on the size of the tumor:
- Stage IIA1: The tumor is 4 centimeters or smaller.
- Stage IIA2: The tumor is larger than 4 centimeters.
- Stage IIB: Cancer has spread from the cervix to the tissue around the uterus.
Learn about treatment of stage II cervical cancer.
Learn about treatment of cervical cancer during pregnancy.
Stage III cervical cancer
In stage III, cervical cancer has spread to the lower third of the vagina and/or to the pelvic wall, and/or has caused kidney problems, and/or involves lymph nodes.
Stage III is subdivided based on how far the cancer has spread.
- Stage IIIA: Cancer has spread to the lower third of the vagina but has not spread to the pelvic wall.
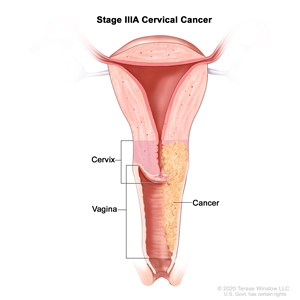
Stage IIIA cervical cancer. Cancer has spread to the lower third of the vagina but has not spread to the pelvic wall. - Stage IIIB: Cancer has spread to the pelvic wall; and/or the tumor has become large enough to block one or both ureters or has caused one or both kidneys to get bigger or stop working.
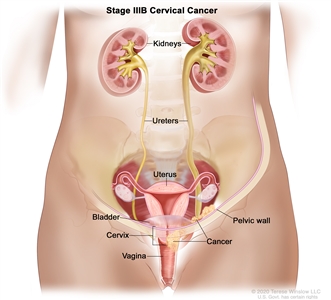
Stage IIIB cervical cancer. Cancer has spread to the pelvic wall and/or the tumor has become large enough to block one or both ureters or has caused one or both kidneys to get bigger or stop working. - Stage IIIC: Stage IIIC is divided into stages IIIC1 and IIIC2, based on the spread of cancer to the lymph nodes.
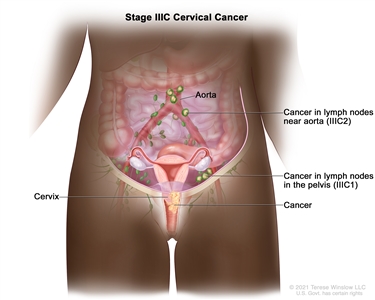
Stage IIIC cervical cancer. In stage IIIC1, cancer has spread to lymph nodes in the pelvis. In stage IIIC2, cancer has spread to lymph nodes in the abdomen near the aorta.
Learn about treatment of stage III cervical cancer.
Learn about treatment of cervical cancer during pregnancy.
Stage IV cervical cancer
In stage IV, cervical cancer has spread beyond the pelvis, or has spread to the lining of the bladder or rectum, or has spread to other parts of the body.
Stage IV is subdivided into stages IVA and IVB, based on where the cancer has spread.
- Stage IVA: Cancer has spread to nearby pelvic organs, such as the bladder or rectum.
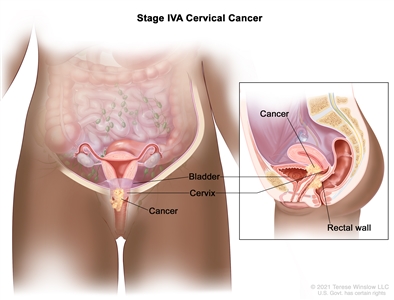
Stage IVA cervical cancer. Cancer has spread to nearby pelvic organs, such as the bladder or rectum. - Stage IVB: Cancer has spread to other parts of the body, such as the liver, lungs, bones, or distant lymph nodes.
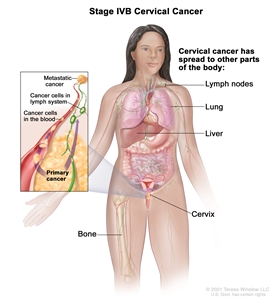
Stage IVB cervical cancer. Cancer has spread to other parts of the body, such as the lymph nodes, lung, liver, or bone.
Stage IV is also called metastatic cancer. Metastatic cancer happens when cancer cells travel through the lymphatic system or blood and form tumors in other parts of the body. The metastatic tumor is the same type of cancer as the primary tumor. For example, if cervical cancer spreads to the lung, the cancer cells in the lung are actually cervical cancer cells. The disease is called metastatic cervical cancer, not lung cancer. Learn more in Metastatic Cancer: When Cancer Spreads.
Learn about treatment options for stage IV cervical cancer.
Learn about treatment of cervical cancer during pregnancy.
Recurrent cervical cancer
Recurrent cervical cancer is cancer that has recurred (come back) after it has been treated. The cancer may come back in the cervix or as metastatic tumors in other parts of the body. Tests will be done to help determine where the cancer has returned in your body, if it has spread, and how far. The type of treatment that you have for recurrent cervical cancer will depend on how far it has spread.
Learn about treatment of recurrent cervical cancer.
Learn more in Recurrent Cancer: When Cancer Comes Back.
Information to help you cope and talk with your health care team is shared in this booklet: When Cancer Returns.
Cervical Cancer Treatment
Different types of treatment are available for cervical cancer. You and your cancer care team will work together to decide your treatment plan, which may include more than one type of treatment. Many factors will be considered, such as the stage of the cancer, your overall health, and your preferences. Your treatment plan will include information about your cancer, the goals of treatment, the treatment options and possible side effects, and the expected length of treatment.
If you are concerned about whether treatment will affect your fertility, talk with your cancer care team before treatment begins about what to expect. To learn about fertility preservation options and ways to find support, visit Fertility Issues in Girls and Women with Cancer.
For information about treatments by stage of cervical cancer, visit Cervical Cancer Treatment by Stage.
For information about treatment during pregnancy, visit Cervical Cancer Treatment during Pregnancy.
Surgery
Surgery (also called an operation) is sometimes used to treat cervical cancer. The type of surgery depends on where the cancer is located. Learn more about Surgery to Treat Cancer.
The following surgical procedures may be used:
Cold knife conization
Cold knife conization uses a scalpel to remove a cone-shaped piece of tissue from the cervix and cervical canal. Sometimes all the cancer can be removed during this procedure. Cold knife conization is done in the hospital under general anesthesia.
Conization may also be used to treat high-grade cervical cell changes.
Sentinel lymph node biopsy
Sentinel lymph node biopsy removes the sentinel lymph node during surgery. The sentinel lymph node is the first lymph node in a group of lymph nodes to receive lymphatic drainage from the primary tumor. It is therefore the first lymph node the cancer is likely to spread to from the primary tumor. To identify the sentinel lymph node, a radioactive substance and/or blue dye is injected near the tumor. The substance or dye flows through the lymph ducts to the lymph nodes. The first lymph node to receive the substance or dye is removed. A pathologist views the tissue under a microscope to look for cancer cells. If cancer cells are found, more lymph nodes will be removed through a separate incision (cut). This is called a lymph node dissection. After the sentinel lymph node biopsy, the surgeon removes the cancer.
Learn more about Sentinel Lymph Node Biopsy.
Hysterectomy
A hysterectomy is surgery to remove the uterus. As a treatment for cervical cancer, the cervix, and sometimes the surrounding structures, are removed. Several types of hysterectomy may be used to treat cervical cancer:
- Total hysterectomy removes the uterus and the cervix. When the surgery is done entirely through the vagina (with no incisions on the abdomen) and the uterus and cervix are removed through the vagina, the operation is called a total vaginal hysterectomy. If the surgery is done through a large incision on the abdomen (either vertical or horizontal) and the uterus and cervix are removed through this incision, the operation is called a total abdominal hysterectomy. If the surgery is done through small incisions on the abdomen, the operation is called a total laparoscopic hysterectomy. The uterus and cervix are usually taken out through the vagina, although sometimes an abdominal incision is made to remove the uterus and cervix.
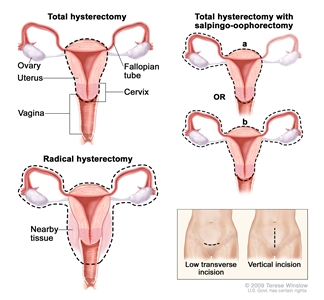
Hysterectomy. The uterus is surgically removed with or without other organs or tissues. In a total hysterectomy, the uterus and cervix are removed. In a total hysterectomy with salpingo-oophorectomy, (a) the uterus plus one (unilateral) ovary and fallopian tube are removed; or (b) the uterus plus both (bilateral) ovaries and fallopian tubes are removed. In a radical hysterectomy, the uterus, cervix, both ovaries, both fallopian tubes, and nearby tissue are removed. These procedures are done using a low transverse incision or a vertical incision. - Radical hysterectomy removes the uterus, cervix, part of the vagina, and a wide area of ligaments and tissues around these organs. The ovaries, fallopian tubes, or nearby lymph nodes may also be removed.
- Modified radical hysterectomy removes the uterus, cervix, upper part of the vagina, and ligaments and tissues that closely surround these organs. This type of surgery removes fewer tissues and/or organs than radical hysterectomy. The ovaries, fallopian tubes, or nearby lymph nodes may also be removed.
Radical trachelectomy
Radical trachelectomy (also called radical cervicectomy) removes the cervix, nearby tissue, and the upper part of the vagina. Lymph nodes may also be removed. After the surgeon removes the cervix, they attach the uterus to the remaining part of the vagina. A special stitch or band is placed on the uterus (in a procedure called a cerclage) to help keep the uterus closed during pregnancy. If you have this surgery, you may still be able to become pregnant.
Bilateral salpingo-oophorectomy
Bilateral salpingo-oophorectomy removes both ovaries and both fallopian tubes. This is done when the cancer has spread to these organs.
Total pelvic exenteration
Total pelvic exenteration removes the lower colon, rectum, and bladder. The cervix, vagina, ovaries, and nearby lymph nodes are also removed. Artificial openings (stoma) are made for urine and stool to flow from the body to a collection bag. Plastic surgery may be needed to make an artificial vagina after this operation.
Radiation therapy
Radiation therapy uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing by damaging their DNA. The two main types of radiation therapy are external radiation therapy and internal radiation therapy (also called brachytherapy).
Both external and internal radiation therapy are used to treat cervical cancer and may also be used as palliative therapy to relieve symptoms and improve quality of life in people with advanced cervical cancer.
External radiation therapy
External beam radiation therapy uses a machine outside the body to send radiation toward the area of the body with cancer. Intensity-modulated radiation therapy (IMRT) is a way of giving external radiation therapy that can help keep radiation from damaging nearby healthy tissue.
IMRT is a type of 3-dimensional (3-D) radiation therapy that uses a computer to make pictures of the size and shape of the tumor. Thin beams of radiation of different intensities (strengths) are aimed directly at the tumor from many angles. IMRT is being studied for the treatment of cervical cancer.
Learn more about External Beam Radiation Therapy for Cancer.
Internal radiation therapy
Internal radiation therapy uses a radioactive substance sealed in needles, seeds, wires, or catheters that are placed directly into or near the cancer. Internal radiation therapy is also called brachytherapy.
Learn more about Brachytherapy to Treat Cancer.
Chemotherapy
Chemotherapy (also called chemo) uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. Chemotherapy may be given alone or with other types of treatment.
Chemotherapy drugs used to treat cervical cancer include:
- cisplatin
- carboplatin
- gemcitabine
- ifosfamide
- irinotecan
- paclitaxel
- topotecan
- vinorelbine
Combinations of these drugs may be used. Other chemotherapy drugs not listed here may also be used.
Learn more about how chemotherapy works against cancer, how it is given, common side effects, and more in Chemotherapy to Treat Cancer.
Targeted therapy
Targeted therapy uses drugs or other substances to block the action of specific enzymes, proteins, or other molecules involved in the growth and spread of cancer cells.
Targeted therapies used to treat cervical cancer include:
- bevacizumab
- tisotumab vedotin
Learn more about how targeted therapy works against cancer, how it is given, possible side effects, and more in Targeted Therapy to Treat Cancer.
Immunotherapy
Immunotherapy helps a person's immune system fight cancer. Biomarker tests can be used to help predict your response to certain immunotherapy drugs. Learn more about Biomarker Testing for Cancer Treatment.
Pembrolizumab is an immunotherapy drug used to treat certain patients whose cervical cancer has the biomarker PD-L1.
Learn more about how immunotherapy works against cancer, how it is given, possible side effects, and more in Immunotherapy to Treat Cancer.
Clinical trials
For some people, joining a clinical trial may be an option. There are different types of clinical trials for people with cancer. For example, a treatment trial tests new treatments or new ways of using current treatments. Supportive care and palliative care trials look at ways to improve quality of life, especially for those who have side effects from cancer and its treatment.
You can use the clinical trial search to find NCI-supported cancer clinical trials accepting participants. The search allows you to filter trials based on the type of cancer, your age, and where the trials are being done. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
Learn more about clinical trials, including how to find and join one, at Clinical Trials Information for Patients and Caregivers.
Follow-up care during and after treatment
As you go through treatment, you will have follow-up tests or checkups. Some of the tests that were done to diagnose cervical cancer or to find out the stage of the cancer may be repeated to see how well the treatment is working. Decisions about whether to continue, change, or stop treatment may be based on the results of these tests.
Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your condition has changed or if the cancer has recurred (come back).
Tell your doctor if you have any of the following signs or symptoms, which may mean the cancer has come back:
- vaginal bleeding or discharge
- pain in the abdomen, back, or leg
- swelling in the leg
- trouble urinating
- change in your bowel movements
- cough
- feeling tired
For cervical cancer, follow-up tests are usually done every 3 to 4 months for the first 2 years, followed by checkups every 6 months. The checkup includes a current health history and exam of the body to check for signs and symptoms of recurrent cervical cancer and for late effects of treatment. A Pap test may or may not be done during your visits.
Learn more about what to expect when treatment ends.
Cervical Cancer Treatment by Stage
The cancer stage (the extent of cancer in the body) is an important factor in deciding the best treatment for cervical cancer. Other factors, such as your preferences and overall health, are also important.
An important factor for some women is fertility preservation. If you would like to retain the ability to become pregnant, ask your doctor about fertility-sparing treatment options (treatments for cervical cancer that preserve the uterus and ovaries). Such treatments may be an option for some small cancers that are only in the cervix. If your cancer is more advanced or has a high chance of coming back, you are more likely to have treatments that will prevent you from becoming pregnant. A reproductive endocrinologist can help you understand your options for becoming a parent, such as freezing eggs. To learn more about fertility preservation options and ways to find support, visit Fertility Issues in Girls and Women with Cancer.
For some people, taking part in a clinical trial may be an option. Clinical trials of new cancer drugs or treatment combinations may be available. Learn more about clinical trials, including how to find and join a trial at Clinical Trials Information for Patients and Caregivers.
Treatment of stage IA cervical cancer
Stage IA cervical cancer is separated into stage IA1 and IA2.
Treatment of stage IA1 cervical cancer may include:
- cold knife conization, a fertility-sparing procedure, for some small cancers
- total hysterectomy with or without bilateral salpingo-oophorectomy, for patients whose cancer has a high risk of coming back
Treatment of stage IA2 cervical cancer may include:
- modified radical hysterectomy and removal of lymph nodes
- radical trachelectomy, a fertility-sparing surgery, and removal of lymph nodes
- internal radiation therapy, for patients who cannot have surgery
To learn more about these treatments, visit Cervical Cancer Treatment.
Treatment of stages IB and IIA cervical cancer
Treatment of stage IB and stage IIA cervical cancer may include:
- radiation therapy given at the same time as chemotherapy
- radical hysterectomy and removal of pelvic lymph nodes with or without radiation therapy to the pelvis, plus chemotherapy
- radical trachelectomy, a fertility-sparing surgery
- radiation therapy alone
- immunotherapy
When radiation is used, it may be given as external radiation therapy only or as a combination of external and internal radiation therapy. Chemotherapy drugs, such as cisplatin or carboplatin, may be given at the same time as radiation therapy. Giving chemotherapy at the same time as radiation therapy helps the radiation therapy work better.
To learn more about these treatments, visit Cervical Cancer Treatment.
Treatment of stages IIB, III, and IVA cervical cancer
Treatment of stage IIB, stage III, and stage IVA cervical cancer may include:
- radiation therapy given at the same time as chemotherapy
- surgery to remove pelvic lymph nodes followed by radiation therapy with or without chemotherapy
- immunotherapy
Most people with stage IIB, III, or IVA cervical cancer will receive a combination of external and internal radiation therapy. Chemotherapy drugs, such as cisplatin or carboplatin, may be given at the same time as radiation therapy. Giving chemotherapy at the same time as radiation therapy helps the radiation therapy work better.
Learn more about these treatments at Cervical Cancer Treatment.
Treatment of stage IVB and recurrent cervical cancer
Treatment of stage IVB and cervical cancer that has recurred (come back) may include:
- The immunotherapy drug pembrolizumab given alone or with other treatments, such as chemotherapy and the targeted therapy drug bevacizumab.
- Radiation therapy and chemotherapy given at the same time, for cancer that has come back in the pelvis. Radiation may be given as external radiation therapy only or as a combination of external and internal radiation therapy. Many different chemotherapy drugs are used to treat recurrent cervical cancer, including cisplatin, carboplatin, ifosfamide, irinotecan, gemcitabine, paclitaxel, topotecan, and vinorelbine. These drugs may be given alone or in combination. Giving chemotherapy at the same time as radiation therapy helps the radiation therapy work better.
- Chemotherapy and bevacizumab as palliative therapy. Many different chemotherapy drugs are used as palliative therapy for recurrent cervical cancer, including cisplatin, carboplatin, ifosfamide, irinotecan, gemcitabine, paclitaxel, topotecan, and vinorelbine. These drugs may be given alone or in combination.
Palliative therapy is treatment meant to improve the quality of life of people who have a serious or life-threatening disease, such as cancer. Many of the same treatments for cancer, such as chemotherapy or other kinds of drugs and radiation therapy, can also be used for palliative therapy to help a patient feel more comfortable. Learn more about Palliative Care in Cancer.
- Pelvic exenteration, for certain people who cannot have radiation therapy. The goal of pelvic exenteration is to cure the cancer by removing it from all the organs to which it has spread.
To learn more about these treatments, visit Cervical Cancer Treatment.
Cervical Cancer Treatment during Pregnancy
Cervical cancer during pregnancy is rare. When it occurs, the cancer is usually found early and confined to the cervix, and it may not need to be treated immediately. But sometimes the cancer is fast-growing or found at a later stage and needs immediate treatment. Before treatment begins, it is important to discuss the benefits and risks of all your treatment options, including how treatment could affect you, your pregnancy, and your future fertility. Your cancer care team will consider your personal wishes when helping you decide the best treatment.
Typically, treatment depends on your trimester of pregnancy.
Treatment of slow-growing stage I cervical cancer in the first trimester
If you have a type of slow-growing cervical cancer that is diagnosed in stage I, are less than 3 months pregnant, and want to continue your pregnancy, your cancer care team might suggest that you delay treatment until later in your pregnancy or after delivery.
Your cancer care team may also suggest you deliver early (around 37 weeks) via cesarean section. You may have a hysterectomy (surgery to remove the uterus and cervix, and sometimes surrounding structures) at the same time as the cesarean section.
To learn more about hysterectomy, see Cervical Cancer Treatment.
Treatment of fast-growing or advanced stage cervical cancer in the first trimester
Tests will be done throughout your pregnancy to find out if the cancer has grown much larger or has spread outside of the cervix. Cervical cancer that is fast-growing or has evidence of spread outside the cervix to other tissues and organs may require immediate treatment, which may include
- hysterectomy, surgery to remove the uterus (womb), cervix, and sometimes surrounding structures
- chemotherapy
- radiation therapy
It is not possible to continue the pregnancy during any of these treatments. Chemotherapy is not safe for the fetus during the first trimester, and radiation therapy is harmful throughout fetal development.
To learn more about these treatments, see Cervical Cancer Treatment.
Treatment of stage I cervical cancer in the second or third trimester
If you are diagnosed with stage I cervical cancer during the second or third trimester of pregnancy, your cancer care team might suggest surgery with cold knife conization or radical trachelectomy.
Cold knife conization uses a scalpel to remove a cone-shaped piece of tissue from the cervix and cervical canal. Cold knife conization is done in the hospital under general anesthesia.
Radical trachelectomy (also called radical cervicectomy) removes the cervix, nearby tissue, and the upper part of the vagina. Lymph nodes may also be removed. After the surgeon removes the cervix, they attach the uterus to the remaining part of the vagina. A special stitch or band is placed on the uterus (in a procedure called a cerclage) to help keep the uterus closed during pregnancy.
Your cancer care team may suggest you deliver early via cesarean section. If all the cancer couldn't be removed with cold knife conization or radical trachelectomy, you may receive other treatments after delivery, such as hysterectomy and radiation therapy.
To learn more about hysterectomy, see Cervical Cancer Treatment.
Treatment of stage II, III, or IV cervical cancer in the second or third trimester
If you are diagnosed with stage II, III, or IV cervical cancer during the second or third trimester of pregnancy, your cancer care team may suggest you continue the pregnancy and receive chemotherapy.
Chemotherapy, such as with cisplatin or carboplatin and paclitaxel, given in the second or third trimester does not usually harm the fetus but may cause early labor and low birth weight.
Your cancer care team may suggest you deliver early via cesarean section so you can receive other treatments, such as hysterectomy and radiation therapy.
Coping with Cervical Cancer
When you first learn that you have cervical cancer, it is normal to feel a mix of emotions. You may wonder how you will cope with the upcoming changes in your life. One step you can take is to be informed of the changes that may occur and what resources are available to help you cope. Doing so can give you a greater sense of control.
Resources on the common physical side effects of treatment for cervical cancer are provided in the Cervical Cancer Treatment section. Learn more about side effects caused by cancer treatment and ways to manage them.
Because cervical cancer tends to occur in people of reproductive age, and because of where it forms in the body, certain aspects of your diagnosis and treatment are of special concern.
Fertility issues
For some people, infertility can be one of the most difficult and upsetting long-term effects of cervical cancer treatment. Although it might feel overwhelming to think about, you may benefit from talking with you doctor about how treatment may affect your fertility and about options to preserve fertility. If you choose to take steps to preserve your fertility, your doctor and a fertility specialist will work together to develop a treatment plan that includes fertility preservation, whenever possible.
Learn more about which cancer treatments may affect fertility and about fertility-sparing treatment options in Fertility Issues in Girls and Women with Cancer.
Sexual problems
Some treatments for cervical cancer can cause short-term or long-term problems with sex after treatment. Sexual problems are often caused by changes to your body. These changes result from chemotherapy, radiation therapy, surgery, or certain medicines.
Learn more about the sexual problems some cancer treatments can cause and ways to cope and share your concerns with your health care team in Sexual Health Issues in Women with Cancer.
Body changes
Cervical cancer and its treatment can change how you look and feel about yourself. Know you aren't alone in how you feel. Coping with these changes can be hard. But, over time, most people learn to adjust to them and move forward.
Learn more about how body changes may affect your self-image and sex life after treatment and ways to cope and communicate your feelings in Self-Image and Sexuality.
Stigma and guilt
Because cervical cancer results from a sexually transmitted infection with human papillomavirus (HPV), you may worry that some people assume your behavior caused your cancer. Or you may blame yourself for lifestyle choices you think could have led to your cancer. It is important to remember almost everyone will have an HPV infection at some point in their lives and that most HPV infections of the cervix will not cause cervical cancer. Having cervical cancer is not your fault. It may help you to share your feelings with someone. Let your doctor know if you would like to talk with a counselor or go to a support group.
Learn more about the emotions many people with cancer feel and ways to cope in Feelings and Cancer and Cancer Support Groups.
Financial toxicity
Cancer is one of the most costly diseases to treat in the United States. You may face major financial challenges and need help dealing with the costs of cervical cancer treatment, even if you have insurance. The problems a person has related to the cost of treatment is known as financial toxicity. Find out if you are at risk and learn about ways to cope in Financial Toxicity (Financial Distress) and Cancer Treatment and Managing Costs and Medical Information.
Last Revised: 2025-04-03
If you want to know more about cancer and how it is treated, or if you wish to know about clinical trials for your type of cancer, you can call the NCI's Cancer Information Service at 1-800-422-6237, toll free. A trained information specialist can talk with you and answer your questions.