Non-Small Cell Lung Cancer Treatment (PDQ®): Treatment - Patient Information [NCI]
This information is produced and provided by the National Cancer Institute (NCI). The information in this topic may have changed since it was written. For the most current information, contact the National Cancer Institute via the Internet web site at http://cancer.gov or call 1-800-4-CANCER.
General Information About Non-Small Cell Lung Cancer
Non-small cell lung cancer is a type of cancer that forms in the tissues of the lung.
The lungs are a pair of cone-shaped breathing organs in the chest. The lungs bring oxygen into the body as you breathe in. They release carbon dioxide, a waste product of the body's cells, as you breathe out. Each lung has sections called lobes. The left lung has two lobes. The right lung is slightly larger and has three lobes. Two tubes called bronchi lead from the trachea (windpipe) to the right and left lungs. Lung cancer may also form in the bronchi. Tiny air sacs called alveoli and small tubes called bronchioles make up the inside of the lungs.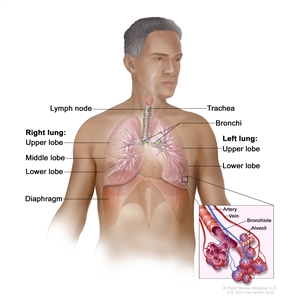
Anatomy of the respiratory system showing the trachea, the right and left lungs and their lobes, and the bronchi. The lymph nodes and the diaphragm are also shown. Oxygen is inhaled into the lungs and passes through the alveoli (the tiny air sacs at the end of the bronchioles) and into the bloodstream (see inset), where it travels to the tissues throughout the body.
A thin membrane called the pleura covers the outside of each lung and lines the inside wall of the chest cavity. This creates a sac called the pleural cavity. The pleural cavity normally contains a small amount of fluid that helps the lungs move smoothly in the chest when you breathe.
There are two main types of lung cancer: non-small cell lung cancer and small cell lung cancer. Non-small cell lung cancer is more common than small cell lung cancer.
There are several types of non-small cell lung cancer.
Each type of non-small cell lung cancer has different kinds of cancer cells. The cancer cells of each type grow and spread in different ways. The types of non-small cell lung cancer are named for the kinds of cells found in the cancer and how the cells look under a microscope:
- Squamous cell carcinoma is a type of lung cancer that forms in the thin, flat cells lining the inside of the lungs. This is also called epidermoid carcinoma.
- Large cell carcinoma is a type of lung cancer that may begin in several types of large cells.
- Adenocarcinoma is a type of lung cancer that begins in the cells that line the alveoli and make substances such as mucus.
Less common types of non-small cell lung cancer include adenosquamous carcinoma, sarcomatoid carcinoma, salivary gland carcinoma, carcinoid tumor, and unclassified carcinoma.
Smoking is the major risk factor for non-small cell lung cancer.
Lung cancer is caused by certain changes to the way lung cells function, especially how they grow and divide into new cells. There are many risk factors for lung cancer, but many do not directly cause cancer. Instead, they increase the chance of DNA damage in cells that may lead to lung cancer. Learn more about how cancer develops at What Is Cancer?
A risk factor is anything that increases the chance of getting a disease. Some risk factors for lung cancer, like smoking, can be changed. However, risk factors also include things you cannot change, like your genetics, age, and family history. Learning about risk factors for lung cancer can help you make changes that might lower your risk of getting it.
Smoking tobacco now or in the past is the most important risk factor for lung cancer. Smoking cigarettes, pipes, or cigars increases the risk of lung cancer. The earlier in life a person starts smoking, the more often a person smokes, and the more years a person smokes, the greater the risk of lung cancer.
Other risk factors for lung cancer include:
- being exposed to secondhand smoke
- being exposed to asbestos, arsenic, chromium, beryllium, nickel, soot, or tar in the workplace
- being exposed to radiation from:
- radiation therapy to the breast or chest
- radon in the home or workplace
- imaging tests such as CT scans
- atomic bomb radiation
- living where there is air pollution
- having a family history of lung cancer
- being infected with HIV
- taking beta carotene supplements and being a heavy smoker
Older age is the main risk factor for most cancers. The chance of getting cancer increases as you get older.
Having one or more of these risk factors does not necessarily mean you will get lung cancer. Many people with risk factors never develop lung cancer, whereas others with no known risk factors do. Talk with your doctor if you think you might be at increased risk.
When smoking is combined with other risk factors, the risk of lung cancer is increased.
Signs and symptoms of non-small cell lung cancer include coughing and shortness of breath.
Sometimes lung cancer does not cause any signs or symptoms. It may be found during a chest x-ray done for another condition. Signs and symptoms may be caused by lung cancer or by other conditions. Check with your doctor if you have:
- chest discomfort or pain
- a cough that doesn't go away or gets worse over time
- trouble breathing
- wheezing
- blood in sputum (mucus coughed up from the lungs)
- hoarseness
- loss of appetite
- weight loss for no known reason
- fatigue
- trouble swallowing
- swelling in the face and/or veins in the neck
Tests that examine the lungs are used to diagnose and stage non-small cell lung cancer.
Non-small cell lung cancer is usually diagnosed with tests and procedures that make pictures of the lung and the area around it. The process used to find out if cancer cells have spread within and around the lung is called staging. Tests and procedures to detect, diagnose, and stage non-small cell lung cancer are usually done at the same time. To plan treatment, it is important to know the stage of the disease and whether the cancer can be removed by surgery.
In addition to asking about your personal and family health history and doing a physical exam, your doctor may perform the following tests and procedures:
- Laboratory tests are medical procedures that test samples of tissue, blood, urine, or other substances in the body. These tests help to diagnose disease, plan and check treatment, or monitor the disease over time.
- Chest x-ray is a type of radiation that can go through the body and make pictures of the organs and bones inside the chest.

A chest x-ray is used to take pictures of the structures and organs inside the chest. X-rays pass through the patient's body onto film or a computer. - CT scan (CAT scan) of the brain, chest, and abdomen uses a computer linked to an x-ray machine to make a series of detailed pictures of areas inside the body. The pictures are taken from different angles and are used to create 3-D views of tissues and organs. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography.
If lung cancer is suspected, you will have a biopsy.
You may have one of the following types of biopsies:
- Fine-needle aspiration (FNA) biopsy of the lung is the removal of tissue or fluid from the lung using a thin needle. A CT scan, ultrasound, or other imaging procedure is used to locate the abnormal tissue or fluid in the lung. A small incision may be made in the skin where the biopsy needle is inserted into the abnormal tissue or fluid. A sample is removed with the needle and sent to the laboratory. A pathologist then views the sample under a microscope to look for cancer cells. A chest x-ray is done after the procedure to make sure no air is leaking from the lung into the chest.
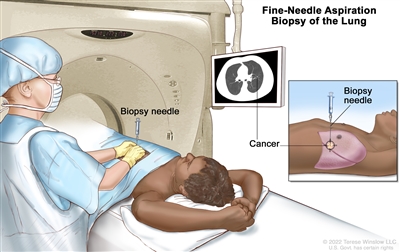
Fine-needle aspiration biopsy of the lung. The patient lies on a table that slides through the computed tomography (CT) machine, which takes x-ray pictures of the inside of the body. The x-ray pictures help the doctor see where the abnormal tissue is in the lung. A biopsy needle is inserted through the chest wall and into the area of abnormal lung tissue. A small piece of tissue is removed through the needle and checked under the microscope for signs of cancer.An endoscopic ultrasound (EUS) is a type of ultrasound that may be used to guide an FNA biopsy of the lung, lymph nodes, or other areas. EUS is a procedure in which an endoscope is inserted into the body. An endoscope is a thin, tube-like instrument with a light and a lens for viewing. A probe at the end of the endoscope is used to bounce high-energy sound waves (ultrasound) off internal tissues or organs and make echoes. The echoes form a picture of body tissues called a sonogram.
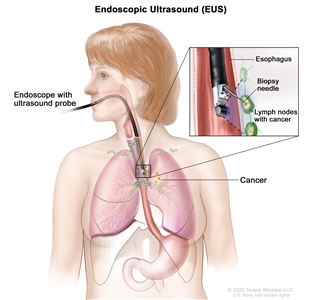
Endoscopic ultrasound-guided fine-needle aspiration biopsy. An endoscope that has an ultrasound probe and a biopsy needle is inserted through the mouth and into the esophagus. The probe bounces sound waves off body tissues to make echoes that form a sonogram (computer picture) of the lymph nodes near the esophagus. The sonogram helps the doctor see where to place the biopsy needle to remove tissue from the lymph nodes. This tissue is checked under a microscope for signs of cancer. - Bronchoscopy is a procedure to look inside the trachea and large airways in the lung for abnormal areas. A bronchoscope is inserted through the nose or mouth into the trachea and lungs. A bronchoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove tissue samples, which are checked under a microscope for signs of cancer.
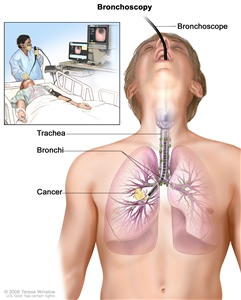
Bronchoscopy. A bronchoscope is inserted through the mouth, trachea, and major bronchi into the lung, to look for abnormal areas. A bronchoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a cutting tool. Tissue samples may be taken to be checked under a microscope for signs of disease. - Thoracoscopy is a surgical procedure to look at the organs inside the chest to check for abnormal areas. An incision (cut) is made between two ribs, and a thoracoscope is inserted into the chest. A thoracoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove tissue or lymph node samples, which are checked under a microscope for signs of cancer. In some cases, this procedure is used to remove part of the esophagus or lung. If certain tissues, organs, or lymph nodes can't be reached, a thoracotomy may be done. In this procedure, a larger incision is made between the ribs and the chest is opened.
- Thoracentesis is the removal of fluid from the space between the lining of the chest and the lung using a needle. A pathologist views the fluid under a microscope to look for cancer cells.
- Mediastinoscopy is a surgical procedure to look at the organs, tissues, and lymph nodes between the lungs for abnormal areas. An incision (cut) is made at the top of the breastbone and a mediastinoscope is inserted into the chest. A mediastinoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove tissue or lymph node samples, which are checked under a microscope for signs of cancer.
- Anterior mediastinotomy is a surgical procedure to look at the organs and tissues between the lungs and between the breastbone and heart for abnormal areas. An incision (cut) is made next to the breastbone and a mediastinoscope is inserted into the chest. A mediastinoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove tissue or lymph node samples, which are checked under a microscope for signs of cancer. This is also called the Chamberlain procedure.
- Lymph node biopsy is the removal of all or part of a lymph node. A pathologist views the lymph node tissue under a microscope to check for cancer cells. A lymph node biopsy may be done at the same time as other types of biopsies.
One or more of the following laboratory tests may be done to study the tissue from the biopsy:
- Molecular tests check for certain genes, proteins, or other molecules in a sample of tissue, blood, or other body fluid. Molecular tests check for certain gene or chromosome changes that occur in non-small cell lung cancer.
- Immunohistochemistry uses antibodies to check for certain antigens (markers) in a sample of a patient's tissue. The antibodies are usually linked to an enzyme or a fluorescent dye. After the antibodies bind to a specific antigen in the tissue sample, the enzyme or dye is activated, and the antigen can then be seen under a microscope. This type of test is used to help diagnose cancer and to help tell one type of cancer from another type of cancer.
After non-small cell lung cancer has been diagnosed, tests are done to find out if cancer cells have spread within the chest or to other parts of the body.
The process used to find out if cancer has spread within the chest or to other parts of the body is called staging. The information gathered from the staging process determines the stage of the disease. It is important to know the stage in order to plan treatment. Some of the tests used to diagnose non-small cell lung cancer are also used to stage the disease.
Imaging tests that may be used in the staging process include:
- MRI (magnetic resonance imaging) of the brain uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the brain. This procedure is also called nuclear magnetic resonance imaging (NMRI).
- PET scan (positron emission tomography scan) uses a small amount of radioactive glucose (sugar) that is injected into a vein. Then a scanner rotates around the body to make detailed, computerized pictures of areas inside the body where the glucose is taken up. Because cancer cells often take up more glucose than normal cells, the pictures can be used to find cancer cells in the body. A PET scan and CT scan may be done at the same time. This is called a PET-CT.
- Bone scan checks for cancer cells in the bone. A very small amount of radioactive material is injected into a vein and travels through the bloodstream. The radioactive material collects in the bones with cancer and is detected by a scanner.
- Pulmonary function test (PFT) checks how well the lungs are working. It measures how much air the lungs can hold and how quickly air moves into and out of the lungs. It also measures how much oxygen is used and how much carbon dioxide is given off during breathing. This is also called lung function test.
- Bone marrow aspiration and biopsy is the removal of bone marrow, blood, and a small piece of bone by inserting a hollow needle into the hipbone or breastbone. A pathologist views the bone marrow, blood, and bone under a microscope to look for signs of cancer.
Some people decide to get a second opinion.
You may want to get a second opinion to confirm your non-small cell lung cancer diagnosis and treatment plan. If you seek a second opinion, you will need to get medical test results and reports from the first doctor to share with the second doctor. The second doctor will review the pathology report, slides, and scans. They may agree with the first doctor, suggest changes or another treatment approach, or provide more information about your cancer.
Learn more about choosing a doctor and getting a second opinion at Finding Cancer Care. You can contact NCI's Cancer Information Service via chat, email, or phone (both in English and Spanish) for help finding a doctor, hospital, or getting a second opinion. For questions you might want to ask at your appointments, visit Questions to Ask Your Doctor About Cancer.
Certain factors affect the prognosis (chance of recovery) and treatment options.
The prognosis and treatment options depend on:
- the stage of the cancer (the size of the tumor and whether it is in the lung only or has spread to other places in the body)
- the type of lung cancer
- whether the cancer has mutations (changes) in certain genes, such as the epidermal growth factor receptor (EGFR) gene or the anaplastic lymphoma kinase (ALK) gene
- whether there are signs and symptoms such as coughing or trouble breathing
- your general health
For most people with non-small cell lung cancer, current treatments do not cure the cancer. If lung cancer is found, you may want to think about taking part in one of the many clinical trials being done to improve treatment or quality of life. Clinical trials are taking place in most parts of the country for people with all stages of non-small cell lung cancer. Information about ongoing clinical trials is available at Clinical Trials Information for Patients and Caregivers.
Stages of Non-Small Cell Lung Cancer
Cancer stage describes the extent of cancer in the body, such as the size of the tumor, whether it has spread, and how far it has spread from where it first formed. It is important to know the stage of non-small cell lung cancer to plan the best treatment.
There are several staging systems for cancer that describe the extent of the cancer. Non-small cell lung cancer staging usually uses the TNM staging system. The cancer may be described by this staging system in your pathology report. Based on the TNM results, a stage (I, II, III, or IV, also written as 1, 2, 3, or 4) is assigned to your cancer. When talking to you about your diagnosis, your doctor may describe the cancer as one of these stages.
Learn about tests to stage non-small lung cell cancer. Learn more about Cancer Staging.
The following stages are used for non-small cell lung cancer:
Occult (hidden) stage non-small cell lung cancer
In the occult (hidden) stage, cancer cannot be seen by imaging or bronchoscopy. Cancer cells are found in sputum or bronchial washings (a sample of cells taken from inside the airways that lead to the lungs). Cancer may have spread to other parts of the body.
Stage 0 (carcinoma in situ)
In stage 0, abnormal cells are found in the lining of the airways. These abnormal cells may become cancer and spread into nearby normal tissue. Stage 0 may be adenocarcinoma in situ (AIS) or squamous cell carcinoma in situ (SCIS).
Stage I (also called stage 1) non-small cell lung cancer
In stage I, cancer has formed. Stage I is divided into stages IA and IB.
- Stage IA:

Stage IA lung cancer. The tumor is in the lung only and is 3 centimeters or smaller. Cancer has not spread to the lymph nodes.The tumor is in the lung only and is 3 centimeters or smaller. Cancer has not spread to the lymph nodes.
- Stage IB:

Stage IB lung cancer. The tumor is larger than 3 centimeters but not larger than 4 centimeters. Cancer has not spread to the lymph nodes; OR the tumor is 4 centimeters or smaller. Cancer has not spread to the lymph nodes and one or more of the following is found: (a) cancer has spread to the main bronchus, but has not spread to the carina; and/or (b) cancer has spread to the inner membrane that covers the lung; and/or (c) part of the lung or the whole lung has collapsed or has pneumonitis (inflammation of the lung).The tumor is larger than 3 centimeters but not larger than 4 centimeters. Cancer has not spread to the lymph nodes.
or
The tumor is 4 centimeters or smaller and one or more of the following is found:
- Cancer has spread to the main bronchus, but has not spread to the carina.
- Cancer has spread to the innermost layer of the membrane that covers the lung.
- Part of the lung or the whole lung has collapsed or has developed pneumonitis.
Cancer has not spread to the lymph nodes.
Stage II (also called stage 2) non-small cell lung cancer
Stage II is divided into stages IIA and IIB.
- Stage IIA:

Stage IIA lung cancer. The tumor is larger than 4 centimeters but not larger than 5 centimeters. Cancer has not spread to the lymph nodes and one or more of the following may be found: (a) cancer has spread to the main bronchus, but has not spread to the carina; and/or (b) cancer has spread to the inner membrane that covers the lung; and/or (c) part of the lung or the whole lung has collapsed or has pneumonitis (inflammation of the lung).The tumor is larger than 4 centimeters but not larger than 5 centimeters. Cancer has not spread to the lymph nodes and one or more of the following may be found:
- Cancer has spread to the main bronchus, but has not spread to the carina.
- Cancer has spread to the innermost layer of the membrane that covers the lung.
- Part of the lung or the whole lung has collapsed or has developed pneumonitis.
- Stage IIB:

Stage IIB lung cancer (1). The primary tumor is 5 centimeters or smaller and cancer has spread to the lymph nodes on the same side of the chest as the primary tumor. The lymph nodes with cancer are in the lung or near the bronchus.The tumor is 5 centimeters or smaller and cancer has spread to lymph nodes on the same side of the chest as the primary tumor. The lymph nodes with cancer are in the lung or near the bronchus. Also, one or more of the following may be found:
- Cancer has spread to the main bronchus, but has not spread to the carina.
- Cancer has spread to the innermost layer of the membrane that covers the lung.
- Part of the lung or the whole lung has collapsed or has developed pneumonitis.
or

Stage IIB lung cancer (2). Cancer has not spread to lymph nodes and one or more of the following is found: (a) the primary tumor is larger than 5 centimeters but not larger than 7 centimeters; and/or (b) there are one or more separate tumors in the same lobe of the lung as the primary tumor; and/or cancer has spread to any of the following: (c) the chest wall and/or the membrane that lines the inside of the chest wall, (d) the nerve that controls the diaphragm, and/or (e) the outer layer of tissue of the sac around the heart.Cancer has not spread to the lymph nodes and one or more of the following is found:
- The tumor is larger than 5 centimeters but not larger than 7 centimeters.
- There are one or more separate tumors in the same lobe of the lung as the primary tumor.
- Cancer has spread to any of the following:
- the membrane that lines the inside of the chest wall
- the chest wall
- the nerve that controls the diaphragm
- the outer layer of tissue of the sac around the heart
Stage III (also called stage 3) non-small cell lung cancer
Stage III is divided into stages IIIA, IIIB, and IIIC.
- Stage IIIA:

Stage IIIA lung cancer (1). The tumor is 5 centimeters or smaller and cancer has spread to lymph nodes on the same side of the chest as the primary tumor. The lymph nodes with cancer are around the trachea or aorta (not shown), or where the trachea divides into the bronchi. Also, one or more of the following may be found: (a) cancer has spread to the main bronchus, but has not spread to the carina; and/or (b) cancer has spread to the inner membrane that covers the lung; and/or (c) part of the lung or the whole lung has collapsed or has pneumonitis (inflammation of the lung).The tumor is 5 centimeters or smaller and cancer has spread to lymph nodes on the same side of the chest as the primary tumor. The lymph nodes with cancer are around the trachea or aorta, or where the trachea divides into the bronchi. Also, one or more of the following may be found:
- Cancer has spread to the main bronchus, but has not spread to the carina.
- Cancer has spread to the innermost layer of the membrane that covers the lung.
- Part of the lung or the whole lung has collapsed or has developed pneumonitis.
or

Stage IIIA lung cancer (2). Cancer has spread to lymph nodes on the same side of the chest as the primary tumor. The lymph nodes with cancer are in the lung or near the bronchus. Also, one or more of the following is found: (a) the tumor is larger than 5 centimeters but not larger than 7 centimeters; and/or (b) there are one or more separate tumors in the same lobe of the lung as the primary tumor; and/or cancer has spread to any of the following: (c) the chest wall and/or the membrane that lines the inside of the chest wall, (d) the nerve that controls the diaphragm, and/or (e) the outer layer of tissue of the sac around the heart.Cancer has spread to lymph nodes on the same side of the chest as the primary tumor. The lymph nodes with cancer are in the lung or near the bronchus. Also, one or more of the following is found:
- The tumor is larger than 5 centimeters but not larger than 7 centimeters.
- There are one or more separate tumors in the same lobe of the lung as the primary tumor.
- Cancer has spread to any of the following:
- the membrane that lines the inside of the chest wall
- the chest wall
- the nerve that controls the diaphragm
- the outer layer of tissue of the sac around the heart
or

Stage IIIA lung cancer (3). Cancer may have spread to lymph nodes on the same side of the chest as the primary tumor. The lymph nodes with cancer are in the lung or near the bronchus. Also, one or more of the following is found: (a) the primary tumor is larger than 7 centimeters; and/or (b) there are one or more separate tumors in a different lobe of the lung with the primary tumor; and/or the tumor is any size and cancer has spread to any of the following: (c) trachea, (d) carina, (e) esophagus, (f) breastbone or backbone, (g) diaphragm, (h) heart, (i) major blood vessels that lead to or from the heart (aorta or vena cava), or the nerve that controls the larynx (not shown).Cancer may have spread to lymph nodes on the same side of the chest as the primary tumor. The lymph nodes with cancer are in the lung or near the bronchus. Also, one or more of the following is found:
- The tumor is larger than 7 centimeters.
- There are one or more separate tumors in a different lobe of the lung with the primary tumor.
- The tumor is any size and cancer has spread to any of the following:
- the trachea
- the carina
- the esophagus
- the breastbone or backbone
- the diaphragm
- the heart
- the major blood vessels that lead to or from the heart (aorta or vena cava)
- the nerve that controls the larynx (voice box)
- Stage IIIB:

Stage IIIB lung cancer (1). The primary tumor is 5 centimeters or smaller and cancer has spread to lymph nodes above the collarbone on the same side of the chest as the primary tumor or to any lymph nodes on the opposite side of the chest as the primary tumor. Also, one or more of the following may be found: (a) cancer has spread to the main bronchus, but has not spread to the carina; and/or (b) cancer has spread to the inner membrane that covers the lung; and/or (c) part of the lung or the whole lung has collapsed or has pneumonitis (inflammation of the lung).The tumor is 5 centimeters or smaller and cancer has spread to lymph nodes above the collarbone on the same side of the chest as the primary tumor or to any lymph nodes on the opposite side of the chest as the primary tumor. Also, one or more of the following may be found:
- Cancer has spread to the main bronchus, but has not spread to the carina.
- Cancer has spread to the innermost layer of the membrane that covers the lung.
- Part of the lung or the whole lung has collapsed or has developed pneumonitis.
or

Stage IIIB lung cancer (2). The tumor may be any size and cancer has spread to lymph nodes on the same side of the chest as the primary tumor. The lymph nodes with cancer are around the trachea or aorta (not shown), or where the trachea divides into the bronchi. Also, one or more of the following is found: (a) there are one or more separate tumors in the same lobe or a different lobe of the lung with the primary tumor; and/or (b) cancer has spread to any of the following: the chest wall or the membrane that lines the inside of the chest wall, the nerve that controls the voice box, the trachea, the carina, the esophagus, the breastbone or backbone (not shown), the diaphragm, the nerve that controls the diaphragm, the heart, the major blood vessels that lead to or from the heart (aorta or vena cava), or the outer layer of tissue of the sac around the heart.The tumor may be any size and cancer has spread to lymph nodes on the same side of the chest as the primary tumor. The lymph nodes with cancer are around the trachea or aorta, or where the trachea divides into the bronchi. Also, one or more of the following is found:
- There are one or more separate tumors in the same lobe or a different lobe of the lung with the primary tumor.
- Cancer has spread to any of the following:
- the membrane that lines the inside of the chest wall
- the chest wall
- the nerve that controls the diaphragm
- the outer layer of tissue of the sac around the heart
- the trachea
- the carina
- the esophagus
- the breastbone or backbone
- the diaphragm
- the heart
- the major blood vessels that lead to or from the heart (aorta or vena cava)
- the nerve that controls the larynx (voice box)
- Stage IIIC:

Stage IIIC lung cancer. The tumor may be any size and cancer has spread to lymph nodes above the collarbone on the same side of the chest as the primary tumor or to any lymph nodes on the opposite side of the chest as the primary tumor. Also, one or more of the following is found: (a) there are one or more separate tumors in the same lobe or a different lobe of the lung with the primary tumor; and/or (b) cancer has spread to any of the following: the chest wall or the membrane that lines the inside of the chest wall, the nerve that controls the voice box, the trachea, the carina, the esophagus, the breastbone or backbone (not shown), the diaphragm, the nerve that controls the diaphragm, the heart, the major blood vessels that lead to or from the heart (aorta or vena cava), or the outer layer of tissue of the sac around the heart.The tumor may be any size and cancer has spread to lymph nodes above the collarbone on the same side of the chest as the primary tumor or to any lymph nodes on the opposite side of the chest as the primary tumor. Also, one or more of the following is found:
- There are one or more separate tumors in the same lobe or a different lobe of the lung with the primary tumor.
- Cancer has spread to any of the following:
- the membrane that lines the inside of the chest wall
- the chest wall
- the nerve that controls the diaphragm
- the outer layer of tissue of the sac around the heart
- the trachea
- the carina
- the esophagus
- the breastbone or backbone
- the diaphragm
- the heart
- the major blood vessels that lead to or from the heart (aorta or vena cava)
- the nerve that controls the larynx (voice box)
Stage IV (also called stage 4) non-small cell lung cancer
Stage IV is divided into stages IVA and IVB.
- Stage IVA:

Stage IVA lung cancer. The tumor may be any size and cancer may have spread to the lymph nodes. One or more of the following is found: (a) there are one or more tumors in the lung that does not have the primary tumor; and/or (b) cancer is found in fluid around the lungs or heart or there are cancer nodules in the lining around the lungs or the sac around the heart; and/or (c) cancer has spread to one place in an organ or tissue not near the lung, such as the brain, adrenal gland, kidney, liver, or bone, or to a lymph node that is not near the lung.The tumor may be any size and cancer may have spread to the lymph nodes. One or more of the following is found:
- There are one or more tumors in the lung that does not have the primary tumor.
- Cancer is found in the lining around the lungs or the sac around the heart.
- Cancer is found in fluid around the lungs or the heart.
- Cancer has spread to one place in an organ not near the lung, such as the brain, liver, adrenal gland, kidney, bone, or to a lymph node that is not near the lung.
- Stage IVB:

Stage IVB lung cancer. The cancer has spread to multiple places in one or more organs that are not near the lung, such as the brain, adrenal gland, kidney, liver, distant lymph nodes, or bone.Cancer has spread to multiple places in one or more organs that are not near the lung.
Non-small cell lung cancer can recur (come back) after it has been treated.
Recurrent non-small cell lung cancer is cancer that has come back after it has been treated. If non-small cell lung cancer comes back, it may come back in the brain, lung, chest, or in other parts of the body. Tests will be done to help determine where the cancer has returned. The type of treatment for non-small cell lung cancer will depend on where it has come back.
Learn more in Recurrent Cancer: When Cancer Comes Back. Information to help you cope and talk with your health care team can be found in the booklet When Cancer Returns.
Treatment Option Overview
There are different types of treatment for people with non-small cell lung cancer.
Different types of treatments are available for people with non-small cell lung cancer. You and your cancer care team will work together to decide your treatment plan, which may include more than one type of treatment. Many factors will be considered, such as the stage of the cancer, your overall health, and your preferences. Your plan will include information about your cancer, the goals of treatment, your treatment options and the possible side effects, and the expected length of treatment.
Talking with your cancer care team before treatment begins about what to expect will be helpful. You'll want to learn what you need to do before treatment begins, how you'll feel while going through it, and what kind of help you will need. To learn more, visit Questions to Ask Your Doctor About Treatment.
The following types of treatment are used:
Surgery
Four types of surgery are used to treat lung cancer:
- Wedge resection is surgery to remove a tumor and some of the normal tissue around it. When a slightly larger amount of tissue is taken, it is called a segmental resection.

Wedge resection of the lung. Part of the lung lobe containing the cancer and a small amount of healthy tissue around it is removed. - Lobectomy is surgery to remove a whole lobe (section) of the lung.

Lobectomy. A lobe of the lung is removed. - Pneumonectomy is surgery to remove one whole lung.

Pneumonectomy. The whole lung is removed. - Sleeve resection is surgery to remove part of the bronchus.
After the doctor removes all the cancer that can be seen at the time of the surgery, some people may be given chemotherapy or radiation therapy after surgery to kill any cancer cells that are left. Treatment given after the surgery to lower the risk that the cancer will come back is called adjuvant therapy.
Radiation therapy
Radiation therapy is a cancer treatment that uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing. There are two types of radiation therapy:
- External radiation therapy uses a machine outside the body to send radiation toward the area of the body with cancer. Certain ways of giving external radiation therapy can help keep radiation from damaging nearby healthy tissue:
- Stereotactic body radiation therapy uses special equipment to ensure you are in the same position for each radiation treatment. Once a day for several days, a radiation machine aims a larger than usual dose of radiation directly at the tumor. By having you in the same position for each treatment, there is less damage to nearby healthy tissue. This procedure is also called stereotactic external beam radiation therapy and stereotaxic radiation therapy.
- Stereotactic radiosurgery is used to treat lung cancer that has spread to the brain. A rigid head frame is attached to the skull to keep the head still during the radiation treatment. A machine aims a single large dose of radiation directly at the tumor in the brain. This procedure does not involve surgery. It is also called stereotaxic radiosurgery, radiosurgery, and radiation surgery.
- Internal radiation therapy uses a radioactive substance sealed in needles, seeds, wires, or catheters that are placed directly into or near the cancer.
For tumors in the airways, radiation is given directly to the tumor through an endoscope.
The way the radiation therapy is given depends on the type and stage of the cancer being treated. It also depends on where the cancer is found. External and internal radiation therapy are used to treat non-small cell lung cancer.
Chemotherapy
Chemotherapy (also called chemo) uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing.
Chemotherapy for non-small cell lung cancer is usually systemic, meaning it is injected into a vein or given by mouth. When given this way, the drugs enter the bloodstream to reach cancer cells throughout the body.
Chemotherapy drugs used to treat non-small cell lung cancer may include:
- carboplatin
- cisplatin
- docetaxel
- doxorubicin
- etoposide
- gemcitabine
- paclitaxel
- pemetrexed
- vinorelbine
Combinations of these chemotherapy drugs may be used. Other chemotherapy drugs not listed here may also be used.
Chemotherapy may also be combined with other kinds of treatment. For example, it may be combined with radiation therapy or immunotherapy drugs.
Learn more about how chemotherapy works, how it is given, common side effects, and more at Chemotherapy to Treat Cancer and Chemotherapy and You: Support for People With Cancer.
Targeted therapy
Targeted therapy uses drugs or other substances to identify and attack specific cancer cells. Your doctor may suggest biomarker tests to help predict your response to certain targeted therapy drugs. Learn more about Biomarker Testing for Cancer Treatment.
Targeted therapies used to treat non-small cell lung cancer include:
- adagrasib
- afatinib
- alectinib
- amivantamab
- bevacizumab
- brigatinib
- capmatinib
- ceritinib
- cetuximab
- crizotinib
- dabrafenib
- dacomitinib
- entrectinib
- erlotinib
- everolimus
- gefitinib
- larotrectinib
- lazertinib
- lorlatinib
- necitumumab
- osimertinib
- pralsetinib
- ramucirumab
- repotrectinib
- selpercatinib
- sotorasib
- tepotinib
- trametinib
Learn more about Targeted Therapy to Treat Cancer.
Immunotherapy
Immunotherapy helps a person's immune system fight cancer. Your doctor may suggest biomarker tests to help predict your response to certain immunotherapy drugs. Learn more about Biomarker Testing for Cancer Treatment.
Immunotherapy drugs used to treat non-small cell lung cancer include:
- atezolizumab
- cemiplimab-rwlc
- durvalumab
- ipilimumab
- nivolumab
- pembrolizumab
- tremelimumab
Learn more about Immunotherapy to Treat Cancer.
Laser therapy
Laser therapy is a cancer treatment that uses a laser beam (a narrow beam of intense light) to kill cancer cells.
Learn more about Lasers to Treat Cancer.
Photodynamic therapy (PDT)
Photodynamic therapy (PDT) is a cancer treatment that uses a drug and a certain type of laser light to kill cancer cells. A drug that is not active until it is exposed to light is injected into a vein. The drug collects more in cancer cells than in normal cells. Fiberoptic tubes are then used to carry the laser light to the cancer cells, where the drug becomes active and kills the cells. Photodynamic therapy causes little damage to healthy tissue. It is used mainly to treat tumors on or just under the skin or in the lining of internal organs. When the tumor is in the airways, PDT is given directly to the tumor through an endoscope.
Learn more about Photodynamic Therapy to Treat Cancer.
Cryosurgery
Cryosurgery is a treatment that uses an instrument to freeze and destroy abnormal tissue, such as carcinoma in situ. This type of treatment is also called cryotherapy. For tumors in the airways, cryosurgery is done through an endoscope.
Learn more about Cryosurgery to Treat Cancer.
Electrocautery
Electrocautery is a treatment that uses a probe or needle heated by an electric current to destroy abnormal tissue. For tumors in the airways, electrocautery is done through an endoscope.
New types of treatment are being tested in clinical trials.
For some people, joining a clinical trial may be an option. There are different types of clinical trials for people with cancer. For example, a treatment trial tests new treatments or new ways of using current treatments. Supportive care and palliative care trials look at ways to improve quality of life, especially for those who have side effects from cancer and its treatment.
You can use the clinical trial search to find NCI-supported cancer clinical trials accepting participants. The search allows you to filter trials based on the type of cancer, your age, and where the trials are being done. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
Learn more about clinical trials, including how to find and join one, at Clinical Trials Information for Patients and Caregivers.
Treatment for non-small cell lung cancer may cause side effects.
For information about side effects caused by treatment for cancer, visit our Side Effects page.
Follow-up care may be needed.
As you go through treatment, you will have follow-up tests or check-ups. Some tests that were done to diagnose or stage the cancer may be repeated to see how well the treatment is working. Decisions about whether to continue, change, or stop treatment may be based on the results of these tests.
Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your condition has changed or if the cancer has recurred (come back).
Treatment of Occult Non-Small Cell Lung Cancer
Treatment of occult non-small cell lung cancer depends on the stage of the disease. Occult tumors are often found at an early stage (the tumor is in the lung only) and sometimes can be cured by surgery.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Stage 0 (carcinoma in situ)
Treatment of stage 0 may include:
- surgery (wedge resection or segmental resection)
- photodynamic therapy, electrocautery, cryosurgery, or laser surgery for tumors in or near the bronchus
Learn more about these treatments in the Treatment Option Overview.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Stage I Non-Small Cell Lung Cancer
Treatment of stage IA non-small cell lung cancer and stage IB non-small cell lung cancer may include:
- surgery (wedge resection, segmental resection, sleeve resection, or lobectomy)
- surgery followed by targeted therapy
- surgery followed by chemotherapy and immunotherapy
- external radiation therapy, including stereotactic body radiation therapy for people who cannot have surgery or choose not to have surgery
Learn more about these treatments and find a list of chemotherapy, targeted therapy, and immunotherapy drugs for lung cancer in the Treatment Option Overview.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Stage II Non-Small Cell Lung Cancer
Treatment of stage IIA non-small cell lung cancer and stage IIB non-small cell lung cancer may include:
- surgery (wedge resection, segmental resection, sleeve resection, lobectomy, or pneumonectomy)
- surgery followed by chemotherapy
- surgery followed by targeted therapy
- surgery followed by chemotherapy and immunotherapy
- surgery followed by immunotherapy
- surgery followed by radiation therapy
- chemotherapy followed by surgery
- immunotherapy and chemotherapy followed by surgery
- immunotherapy and chemotherapy followed by surgery and more immunotherapy
- external radiation therapy for people who cannot have surgery
Learn more about these treatments and find a list of chemotherapy, targeted therapy, and immunotherapy drugs for lung cancer in the Treatment Option Overview.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Stage IIIA Non-Small Cell Lung Cancer
Treatment of stage IIIA non-small cell lung cancer that can be removed with surgery may include:
- chemotherapy followed by surgery
- chemotherapy and radiation therapy followed by surgery
- immunotherapy and chemotherapy followed by surgery
- immunotherapy and chemotherapy followed by surgery and more immunotherapy
- surgery followed by chemotherapy
- surgery followed by targeted therapy
- surgery followed by chemotherapy and immunotherapy
- surgery followed by immunotherapy
- surgery followed by chemotherapy and radiation therapy
- surgery followed by radiation therapy
Treatment of stage IIIA non-small cell lung cancer that cannot be removed with surgery may include:
- chemotherapy and radiation therapy
- chemotherapy and radiation therapy followed by immunotherapy
- external radiation therapy alone
- internal radiation therapy or laser surgery as palliative treatment to relieve symptoms and improve quality of life
Learn more about supportive care for signs and symptoms including cough, shortness of breath, and chest pain at Cardiopulmonary Syndromes and Cancer Pain.
Non-small cell lung cancer of the superior sulcus, often called Pancoast tumor, begins in the upper part of the lung and spreads to nearby tissues such as the chest wall, large blood vessels, and spine. Treatment of Pancoast tumors may include:
- surgery
- chemotherapy and radiation therapy followed by surgery
- radiation therapy alone
Some stage IIIA non-small cell lung tumors that have grown into the chest wall may be completely removed. Treatment of chest wall tumors may include:
- surgery
- surgery and radiation therapy
- radiation therapy alone
- chemotherapy combined with radiation therapy and/or surgery
Learn more about these treatments and find a list of chemotherapy drugs for lung cancer in the Treatment Option Overview.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Stage IIIB and Stage IIIC Non-Small Cell Lung Cancer
Treatment of stage IIIB non-small cell lung cancer and stage IIIC non-small cell lung cancer may include:
- chemotherapy followed by external radiation therapy
- chemotherapy with radiation therapy
- immunotherapy and chemotherapy followed by surgery and more immunotherapy
- immunotherapy before or after chemotherapy and radiation therapy
- targeted therapy before or after chemotherapy and radiation therapy
- external radiation therapy alone for people who cannot have chemotherapy
- external radiation therapy as palliative therapy to relieve symptoms and improve quality of life
- laser therapy and/or internal radiation therapy to relieve symptoms and improve quality of life
Learn more about these treatments and find a list of chemotherapy, targeted therapy, and immunotherapy drugs for lung cancer in the Treatment Option Overview.
Learn more about supportive care for signs and symptoms such as cough, shortness of breath, and chest pain at Cardiopulmonary Syndromes and Cancer Pain.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Newly Diagnosed Stage IV, Relapsed, and Recurrent Non-Small Cell Lung Cancer
Treatment of newly stage IV, relapsed, and recurrent non-small cell lung cancer may include:
- one or more chemotherapy drugs with or without targeted therapy
- combination chemotherapy followed by more chemotherapy as maintenance therapy to help keep cancer from progressing
- targeted therapy
- one or more immunotherapy drugs
Learn more about these treatments and find a list of chemotherapy, targeted therapy, and immunotherapy drugs for lung cancer in the Treatment Option Overview.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Progressive Stage IV, Relapsed, and Recurrent Non-Small Cell Lung Cancer
Treatment of progressive stage IV, relapsed, and recurrent non-small cell lung cancer may include:
- chemotherapy
- targeted therapy with or without chemotherapy
- immunotherapy
Learn more about these treatments and find a list of chemotherapy, targeted therapy, and immunotherapy drugs for lung cancer in the Treatment Option Overview.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
To Learn More About Non-Small Cell Lung Cancer
For more information from the National Cancer Institute about non-small cell lung cancer, visit:
- Lung Cancer Home Page
- Lung Cancer Prevention
- Lung Cancer Screening
- Drugs Approved for Non-Small Cell Lung Cancer
- Tobacco (includes help with quitting)
- Secondhand Smoke and Cancer
For general cancer information and other resources from the National Cancer Institute, visit:
About This PDQ Summary
About PDQ
Physician Data Query (PDQ) is the National Cancer Institute's (NCI's) comprehensive cancer information database. The PDQ database contains summaries of the latest published information on cancer prevention, detection, genetics, treatment, supportive care, and complementary and alternative medicine. Most summaries come in two versions. The health professional versions have detailed information written in technical language. The patient versions are written in easy-to-understand, nontechnical language. Both versions have cancer information that is accurate and up to date and most versions are also available in Spanish.
PDQ is a service of the NCI. The NCI is part of the National Institutes of Health (NIH). NIH is the federal government's center of biomedical research. The PDQ summaries are based on an independent review of the medical literature. They are not policy statements of the NCI or the NIH.
Purpose of This Summary
This PDQ cancer information summary has current information about the treatment of non-small cell lung cancer. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Reviewers and Updates
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary ("Updated") is the date of the most recent change.
The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Adult Treatment Editorial Board.
Clinical Trial Information
A clinical trial is a study to answer a scientific question, such as whether one treatment is better than another. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in order to find new and better ways to help cancer patients. During treatment clinical trials, information is collected about the effects of a new treatment and how well it works. If a clinical trial shows that a new treatment is better than one currently being used, the new treatment may become "standard." Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Clinical trials can be found online at NCI's website. For more information, call the Cancer Information Service (CIS), NCI's contact center, at 1-800-4-CANCER (1-800-422-6237).
Permission to Use This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely as text. It cannot be identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as "NCI's PDQ cancer information summary about breast cancer prevention states the risks in the following way: [include excerpt from the summary]."
The best way to cite this PDQ summary is:
PDQ® Adult Treatment Editorial Board. PDQ Non-Small Cell Lung Cancer Treatment. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/types/lung/patient/non-small-cell-lung-treatment-pdq. Accessed <MM/DD/YYYY>. [PMID: 26389355]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use in the PDQ summaries only. If you want to use an image from a PDQ summary and you are not using the whole summary, you must get permission from the owner. It cannot be given by the National Cancer Institute. Information about using the images in this summary, along with many other images related to cancer can be found in Visuals Online. Visuals Online is a collection of more than 3,000 scientific images.
Disclaimer
The information in these summaries should not be used to make decisions about insurance reimbursement. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website's E-mail Us.
Last Revised: 2025-03-28
If you want to know more about cancer and how it is treated, or if you wish to know about clinical trials for your type of cancer, you can call the NCI's Cancer Information Service at 1-800-422-6237, toll free. A trained information specialist can talk with you and answer your questions.