Lumbar Herniated Disc
Condition Basics
What is a herniated disc?
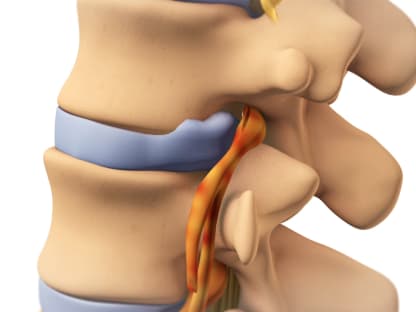
The bones (vertebrae) that form the spine in your back are cushioned by small, spongy discs. When these discs are healthy, they act as shock absorbers for the spine and keep the spine flexible. But when a disc is damaged, it may bulge or break open. This is called a herniated disc. It may also be called a slipped or ruptured disc.
You can have a herniated disc in any part of your spine. But most herniated discs affect the lower back (lumbar herniated disc). Some happen in the neck (cervical herniated disc). Less often, they can be in the upper back (thoracic herniated disc).
What causes it?
A herniated disc usually is caused by wear and tear. As we age, the discs in our spine lose some of the fluid that keeps them flexible. It also may be caused by an injury to the spine. The injury may cause tiny tears or cracks on the outside of the disc.
What are the symptoms?
If a lumbar herniated disc isn't pressing on a nerve, you may have an ache in your low back. Or you may have no symptoms at all. If the disc irritates or presses on the nerve, symptoms include pain, numbness, and weakness in the buttock and down the leg.
How is it diagnosed?
Your doctor may diagnose a herniated disc by asking questions about your symptoms and examining you. You may not need tests. But your doctor may do tests such as an MRI or a CT scan to confirm a herniated disc or rule out other health problems.
How is a lumbar herniated disc treated?
Usually symptoms from a herniated disc will get better on their own. So most people try nonsurgical treatment first. This includes taking over-the-counter pain medicines, using heat or ice, and doing suggested exercises. Some people take part in physical therapy or rehabilitation programs. If symptoms don't get better, surgery may be an option.
Health Tools
Health Tools help you make wise health decisions or take action to improve your health.
Cause
Wear and tear, also called disc degeneration, is the usual cause of a herniated disc. As we age, the discs in our spine lose some of the fluid that helps them stay flexible. The outer layer of the discs can form tiny tears or cracks. The thick gel inside the disc may be forced out through those cracks and cause the disc to bulge or break open.
A herniated disc can occur from:
- A sudden, heavy strain or increased pressure to the lower back. Sometimes a sudden twisting movement or even a sneeze will force some of the material out.
- Activities that are done over and over again that may stress the lower back. Examples include poor lifting habits, being exposed to vibration for a long time, and sports-related injuries.
Learn more
What Increases Your Risk
You may not always be able to prevent a herniated disc from happening. But there may be some things that make it more likely to happen. Things that make it more likely you'll get a herniated disc are called risk factors.
Risk factors may include:
- Getting older.
- Having a history of back injury, previous herniated disc, or back surgery.
- Your job or other activities. These may include things like:
- Lifting or pulling heavy objects.
- Bending or twisting the back often.
- Your exercise habits, such as:
- Not exercising regularly.
- Smoking. Nicotine and other toxins from smoking can keep your spinal discs from absorbing all the nutrients they need from the blood. This can make an injured disc more likely.
- Being overweight.
Prevention
You may not always be able to prevent a herniated disc from happening. But there are some things you can try that may help.
- Stay at a healthy body weight. This may reduce the load on your lower back.
- Get regular exercise to help keep your core muscles strong.
- Use proper lifting techniques.
- Lift with your legs (not your back) by squatting and bending your knees. Avoid bending forward at the waist.
- Keep the load as close to your body as possible, at the level of your belly button.
- Avoid turning or twisting your body while holding a heavy object.
- Quit smoking. Nicotine can harm the discs in your back, because it makes the discs less able to absorb the nutrients they need to stay healthy. And it may cause the discs to become dry and brittle.
Learn more
Watch
Symptoms
Many people with herniated discs have no symptoms. Pain happens when the bulging disc irritates the membrane on the outside of the spinal nerves. If the disc irritates or presses on the nerve roots in the spine, it can cause weakness or numbness in the area of the body where that nerve travels. If the herniated disc isn't pressing on a nerve, you may have an ache in your low back.
When the disc irritates or presses on a nerve in the lower back, symptoms may include:
- Pain that travels through the buttock and down a leg to the ankle or foot because of pressure on the sciatic nerve. There may also be low back pain.
- Tingling or numbness in one leg. It can start in the buttock or behind the knee and extend to the thigh, ankle, or foot.
- Pain in the front of the thigh.
- Severe deep muscle pain and muscle spasms.
Weakness in both legs and the loss of bladder or bowel control are symptoms of a specific and severe type of nerve root compression called cauda equina syndrome. This is a rare but serious problem. A person with these symptoms should see a doctor right away.
What Happens
Age or injury can cause the outer layer of a spinal disc to dry out and form tiny cracks. Sometimes this causes a disc to herniate. This can happen in several ways. They include a:
- Bulging disc. The disc may start to bulge out from between the bones of the spine (vertebrae).
- Ruptured disc. The gel breaks through the capsule. The thick gel inside the disc is forced out through the cracks and causes the disc to break open.
- Free fragment. Fragments of a ruptured disc may break completely free of the disc and get stuck in the spinal canal.
Any of these can cause irritation or pressure on a nerve root and symptoms of pain and numbness.
Symptoms usually fade over time as your body reabsorbs the herniated disc material. Most people who have a herniated disc notice their symptoms improving over several weeks.
When to Call a Doctor
Call 911 or other emergency services immediately if:
- An injury causes numbness or weakness in one or both legs.
Call your doctor now if:
- You have a new loss of bowel or bladder control.
- You have leg pain along with persistent weakness, tingling, or numbness in any part of the leg from the buttock to the ankle or foot.
- You have low back pain along with vomiting, fever, or both.
- Leg pain or intermittent weakness, tingling, or numbness lasts longer than 1 week despite home treatment.
- You have back pain that either won't go away or builds in intensity over a few weeks.
- You have a back injury, and your symptoms don't improve in 2 to 3 days.
- You have back pain along with pain during urination or blood in the urine.
- You have back pain that is worse when you are resting than when you are active.
- You notice a gradual increase in problems with bowel or bladder control.
Watchful waiting
Watchful waiting is a wait-and-see approach. If you get better on your own, you won't need treatment. If you get worse, you and your doctor will decide what to do next.
If you have pain, numbness, or tingling in one leg that gets worse with sitting, standing, or walking (without any obvious leg weakness):
- You may try a brief period of bed rest—usually no more than 1 to 2 days—then gradually begin activities if the pain is manageable.
- Take short walks.
- Avoid movements and positions that increase pain or numbness.
Exams and Tests
To find out if you have a herniated disc, your doctor will ask you questions about your symptoms and do an exam. If this suggests that you have a herniated disc, you probably won't need other tests. But if your doctor needs more information, you may have an MRI or a CT scan. Your doctor may order one of these if:
- Your medical history and physical exam suggest a more serious condition. (This could include a tumor, an infection, or severe nerve damage.)
- Your leg pain and other symptoms don't get better after 6 weeks of nonsurgical treatment.
Other tests, such as blood tests, may be done to rule out other conditions.
Some tests are done to give your doctor more information. They aren't used as often as an MRI or a CT scan. These tests may include:
- An electromyogram and nerve conduction test.
- A myelogram.
- A nerve block.
Learn more
Watch
Treatment Overview
Usually, symptoms from a herniated disc will get better on their own. So most people try nonsurgical treatment first.
Treatment may include:
- Home care. This includes avoiding activities and positions that make pain worse, taking short walks, and using heat or ice if they make you feel better.
- Doing exercises that your doctor or physical therapist suggests. These may include core stabilization exercises, which can help you strengthen the muscles of your trunk to protect your back.
- Taking medicines to treat your symptoms, if your doctor says it's okay. Medicines such as NSAIDs (ibuprofen, naproxen) or acetaminophen are usually tried first. Other medicines that are sometimes tried include stronger pain medicines or muscle relaxers. Steroid shots are also sometimes used.
Some people take part in pain management programs, physical therapy (PT), or rehabilitation programs.
Surgery
Surgery can be a good choice for people who have nerve damage that is getting worse. Or it can be good choice for people who have pain that hasn't improved after at least 6 weeks of nonsurgical treatment. Only a few people have enough pain to consider surgery.
The most common surgery for herniated disc is discectomy. Many people are able to go back to work and daily activities quickly. In some cases, your doctor may recommend PT and home exercises after your surgery.
Learn more
Self-Care
Symptoms from a herniated disc usually get better in a few weeks or months. Here are steps to reduce pain and strengthen your back.
- Ease back into daily activities.
For the first day or two of pain, take it easy. But as soon as possible, ease back into your normal daily life and activities. When a movement hurts, go gently.
- Rest if you have severe pain.
Otherwise, stay active. Your doctor may recommend a short period of rest or reduced activity followed by a gradual increase in activity. Lying down for too long can make back pain worse. Sitting can make it worse too.
- When you rest, find a comfortable position.
You might prefer lying on the floor or a medium-firm bed with a small pillow under your head and another under your knees. Or you can try lying on your side with a pillow between your knees. Don't stay in one position for too long. When you're resting, change positions every 30 minutes.
- Take a short walk.
Walk for 10 to 20 minutes on a level surface (no slopes, hills, or stairs) every 2 to 3 hours. Walk only distances you can manage without pain, especially leg pain.
- Use heat or ice for pain.
There is not strong evidence that either heat or ice will help, but you can try them to see if they help you. You may also want to try switching between heat and cold.
- Do exercises that your doctor or physical therapist suggests.
These will help keep your back muscles strong and prevent another injury.
- Don't smoke.
Smoking increases the risk of a disc injury.
Learn more
Watch
Medicines
Medicine doesn't cure a herniated disc. But it may reduce inflammation and pain and allow you to start an exercise program to strengthen your stomach and back muscles. Medicines include:
- Pain relievers. These include acetaminophen (such as Tylenol) and nonsteroidal anti-inflammatory drugs (NSAIDs). NSAIDs include ibuprofen (such as Advil) and naproxen (such as Aleve).
- Muscle relaxants.
- Corticosteroids.
- Opioids.
Learn more
Watch
Surgery
Emergency surgery is done if a herniated disc causes cauda equina syndrome. Signs include:
- New loss of bowel or bladder control.
- New weakness in the legs (usually both legs).
- New numbness or tingling in the buttocks, genital area, or legs (usually both legs).
Surgery may be an option if:
- You have leg pain that hasn't improved with at least 6 weeks of nonsurgical treatment, you take strong pain medicine for your symptoms, and your symptoms are bad enough to interfere with normal activities and work.
- The nerve that the herniated disc is pressing on is causing weakness, loss of motion, or abnormal sensitivity in the area of the body that the nerve controls.
- Tests show that your herniated disc can be treated surgically.
Back surgery may relieve your pain faster than nonsurgical treatments. But over time, surgery and nonsurgical treatments work about the same to reduce pain and other symptoms.footnote 1, footnote 2 Some people need more disc surgery after their first surgery.
Many people are able to slowly get back to work and daily activities soon after surgery. In some cases, your doctor may recommend a rehabilitation program after surgery. It might include physical therapy and home exercises.
Disc surgery isn't thought to be an effective treatment for low back pain that is not caused by a herniated disc. Disc surgery is also not done if back pain is the only symptom that the herniated disc causes.
Surgery choices
There are different ways to remove disc material. They are:
- Open discectomy. This is done through a large cut, called an incision, in your back.
- Microdiscectomy. This is done through a smaller incision. It causes less damage to surrounding tissue.
- Minimally invasive procedures. These are done through one or more tiny incisions in your back. Your doctor can put special tools through the incisions, such as cutting or heating devices or lasers. These tools can cut or destroy part of the disc.
Studies haven't shown noticeable differences in how well each of these procedures works.footnote 3 So you and your doctor will think about several things in deciding which treatment may be right for you. These include your own body structure, your symptoms, which disc is herniated, what you prefer, and your doctor's expertise and experience.
In some cases, a small piece of bone from the affected vertebra may be removed. This small piece is called the lamina. It's the thin part of the vertebrae that forms a protective arch over the spinal cord. A procedure called a laminotomy removes some of the lamina. A laminectomy removes most of or all of the lamina. It also may remove thickened tissue that is narrowing the spinal canal. Either of these procedures may be done at the same time as a discectomy. Or they may be done separately.
Learn more
Watch
Complementary Treatments
Some people use complementary medicine along with standard medical care to treat leg and back pain caused by a herniated disc. Some examples are acupuncture, manipulation of the spine, and massage. Talk to your doctor before using complementary medicine to treat a herniated disc.
Learn more
References
Citations
- Peul WC, et al. (2007). Surgical versus prolonged conservative treatment for sciatica. New England Journal of Medicine, 356(22): 2245–2256.
- Weinstein JN, et al. (2008). Surgical versus nonoperative treatment for lumbar disc herniation: Four-year results for the Spine Patient Outcomes Research Trial (SPORT). Spine, 33(25): 2789–2800. DOI: 10.1097/BRS.0b013e31818ed8f4. Accessed November 18, 2015.
- Rasouli MR, et al. (2014). Minimally invasive discectomy versus microdiscectomy/open discectomy for symptomatic lumbar disc herniation. Cochrane Database of Systematic Reviews (9). DOI: 10.1002/14651858.CD010328.pub2. Accessed October 15, 2015.
Credits
Current as of: July 24, 2025
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: July 24, 2025
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.